Nerve transfers in the forearm and wrist are devised to restore forearm and wrist function through reinnervation of target muscles. The available nerve transfers for the forearm and wrist are procedures to restore forearm pronation/supination and wrist flexion/extension function. Of these functions, restoration of pronation is the most emphasized within this region. Majority of nerve transfers that assist in wrist flexion/extension can be found in the Hand Section as the muscles targeted for reinnervation cross the wrist for a distal attachment and assist in wrist function. Motor nerve transfers are time sensitive due to muscle atrophy and loss of motor end-plates.
Procedures – Restoration of Forearm and Wrist Function
Forearm Pronation
Wrist Extension
Title: Median (FCR / FDS) to Radial (PIN / ECRB) Nerve Transfer.
Published: 7/14/2011, Updated: 7/19/2011.
Author(s): Ida K. Fox MD, Andrew Yee BS, Susan E. Mackinnon MD.
Division of Plastic and Reconstructive Surgery, Washington University School of Medicine, St. Louis, MO.
The median to radial nerve transfer was first performed in a unique radial nerve palsy patient. This first patient had a proximal injury associated with a humeral head fracture and lost radial nerve function. In this case, tendon transfers were contraindicated due to coexisting complex regional pain syndrome and associated stiffness. In addition, nerve grafting was contraindicated due to proximal level of injury and advanced age. Excellent results following the median to radial nerve transfer in this single patient have allowed the expansion of indications such that nerve transfers are an alternative to tendon transfers and nerve grafting. The median to radial nerve transfer utilizes the following specific nerve branches for transfer: (1) flexor carpi radialis to the posterior interosseous nerve and (2) flexor digitorum superficialis to the extensor carpi radialis brevis. The median nerve branches are “pre-dissected” and no interfascicular dissection is required during this procedure. At our institution, we combine this with an end-to-side tendon transfer of pronator teres to extensor carpi radialis brevis as long as there is no significant stiffness for early recovery of wrist extension. Early motor re-education shortens the time of recovery, with reinnervation of radial nerve muscles usually noted by nine months.
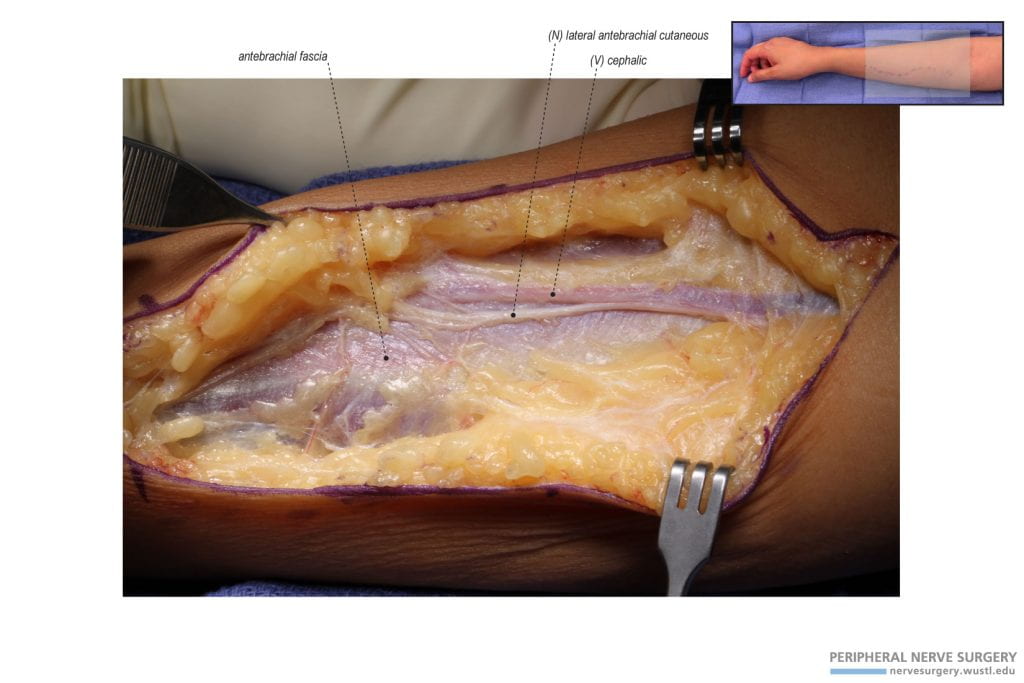
Figure 1 – Orientation and incision for median to radial nerve transfer. A lazy-S incision is made over the proximal volar forearm, starting in the antecubital fossa and extending half of the distance to the wrist crease over the medial border of the brachioradialis. The incision has been lengthened distally to mobilize the pronator teres tendon for transfer to the extensor carpi radialis tendon. (A) Orientation image and dotted markings for an unused incision. (B) Actual incision is visualized.
Figure 2 – Exposure and identification of the lateral antebrachial cutaneous nerve (LABC). Upon exposure, the LABC is identified to accompany the cephalic or accessory cephalic vein. These structures are protected as dissection continues through the antebrachial fascia.
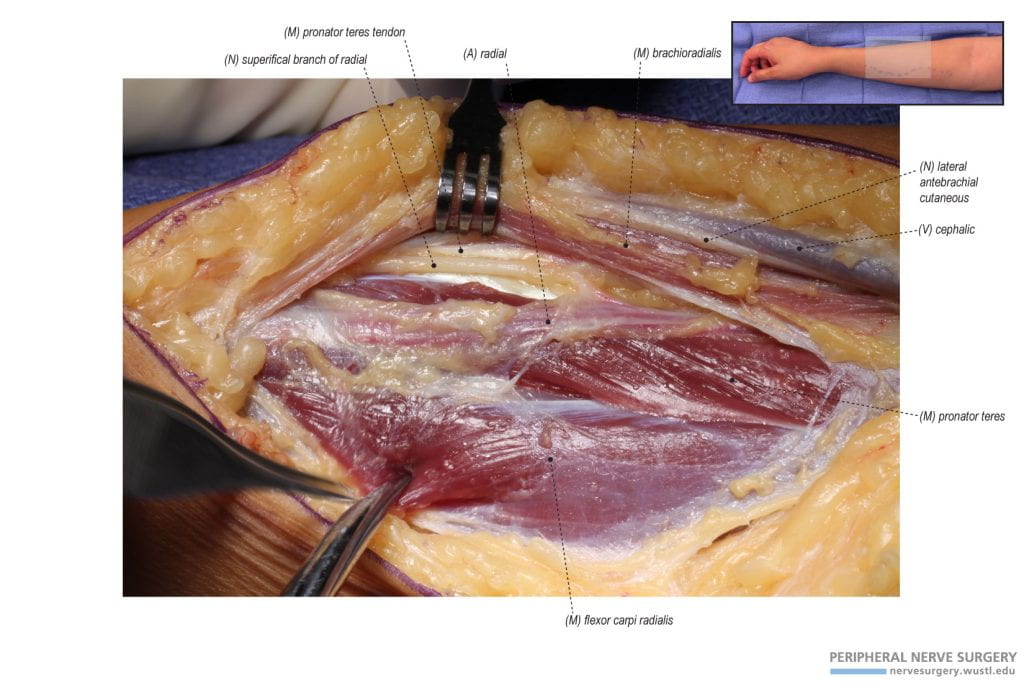
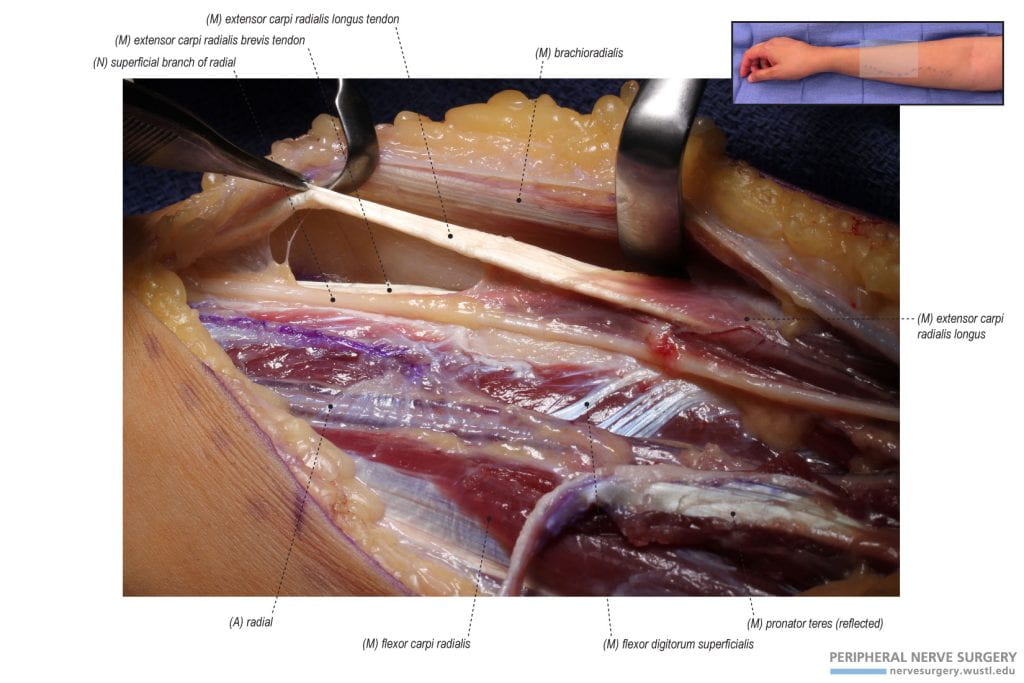
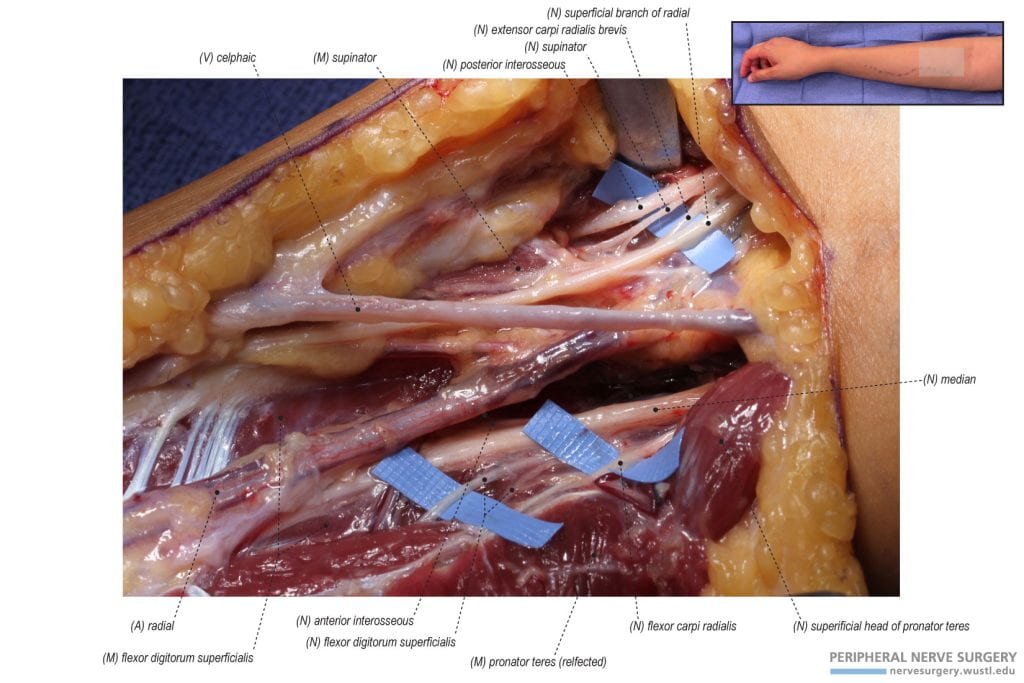
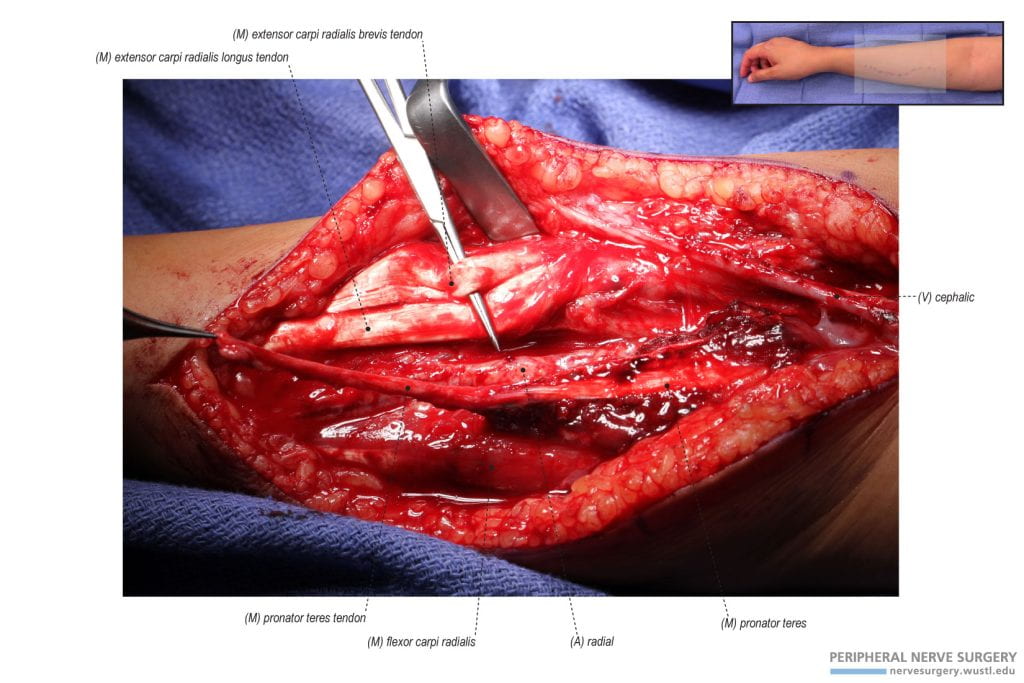
Figure 3 – Landmarks for identifying the tendon of the superficial head of the pronator teres. radial vessels, specifically the radial artery, are found between the brachioradialis and the pronator teres. By retracting the brachioradialis laterally, the superficial branch of the radial nerve is identified lateral to the radial vessels. Lateral to this nerve or beneath lies the tendon of the superficial head of the pronator teres.
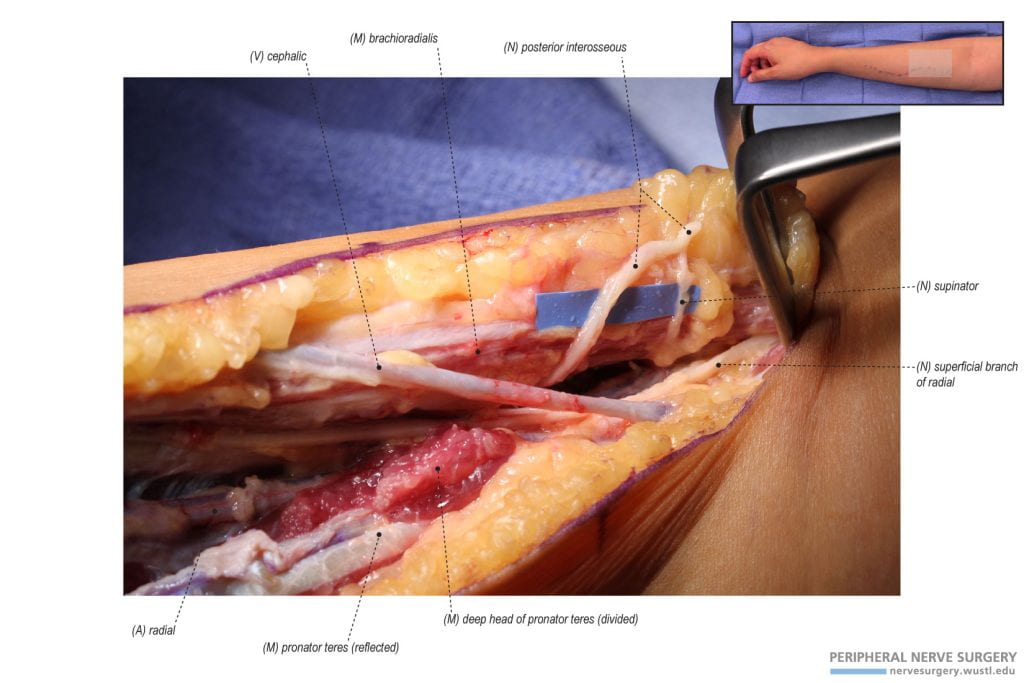
Figure 4 – Identifying the tendon of the superficial head of the pronator teres to release for the pronator teres (PT) to extensor carpi radialis brevis (ECRB) tendon transfer. The pronator teres tendon is marked in purple to mobilize and release it from the radius for the PT to ECRB tendon transfer. However, if this tendon transfer is not performed unlike in his case, the pronator teres tendon is step-lengthened with a “Z-like” incision to allow for the proximal exposure of the median nerve for transfer.
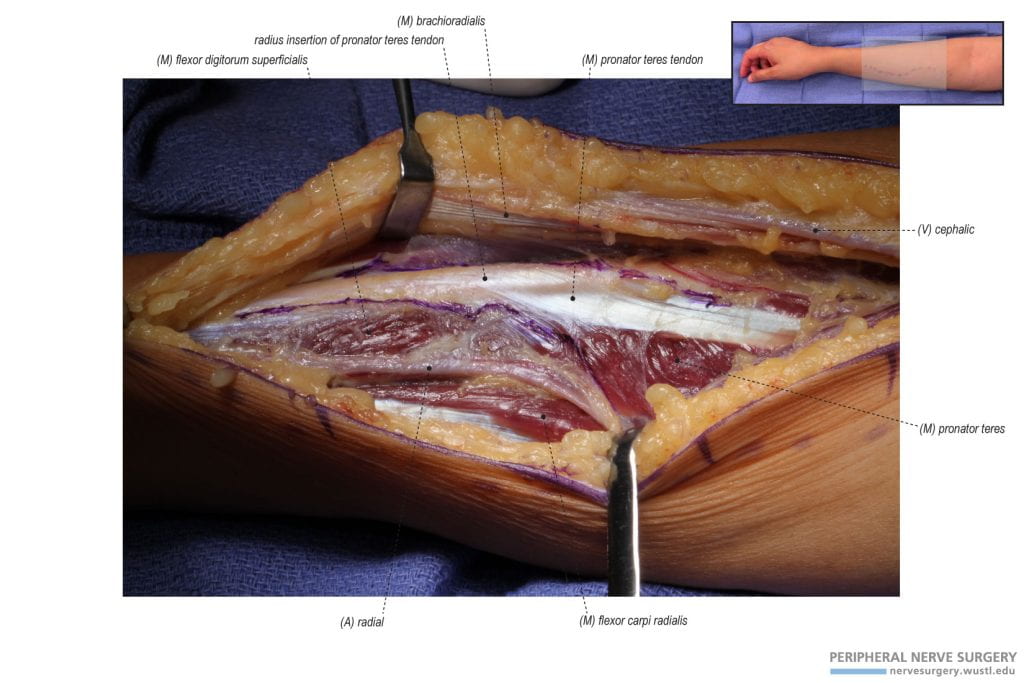
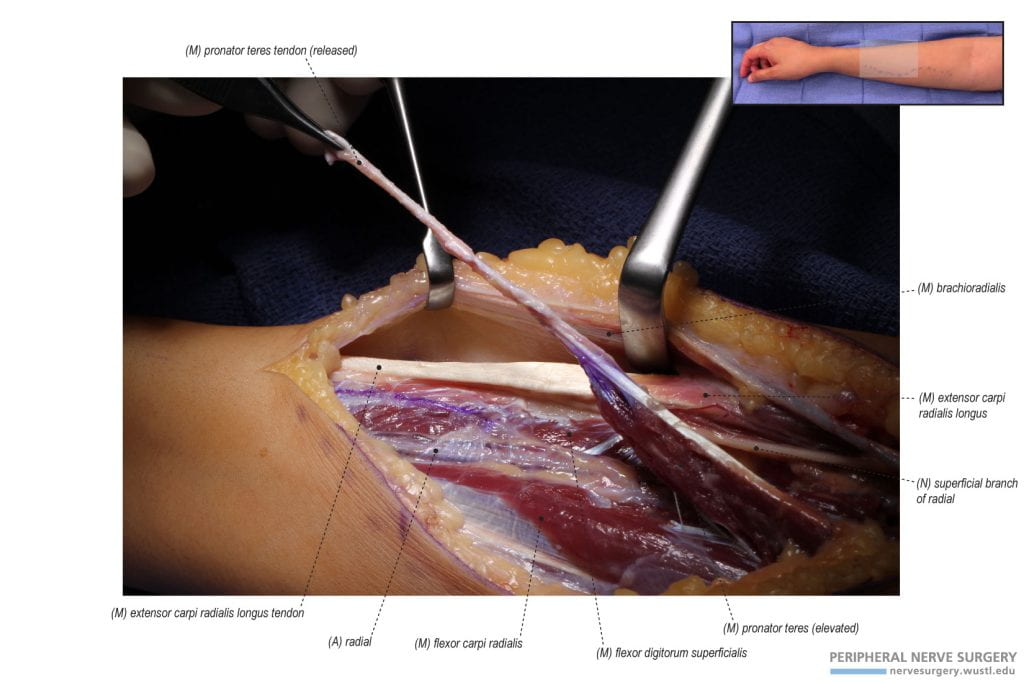
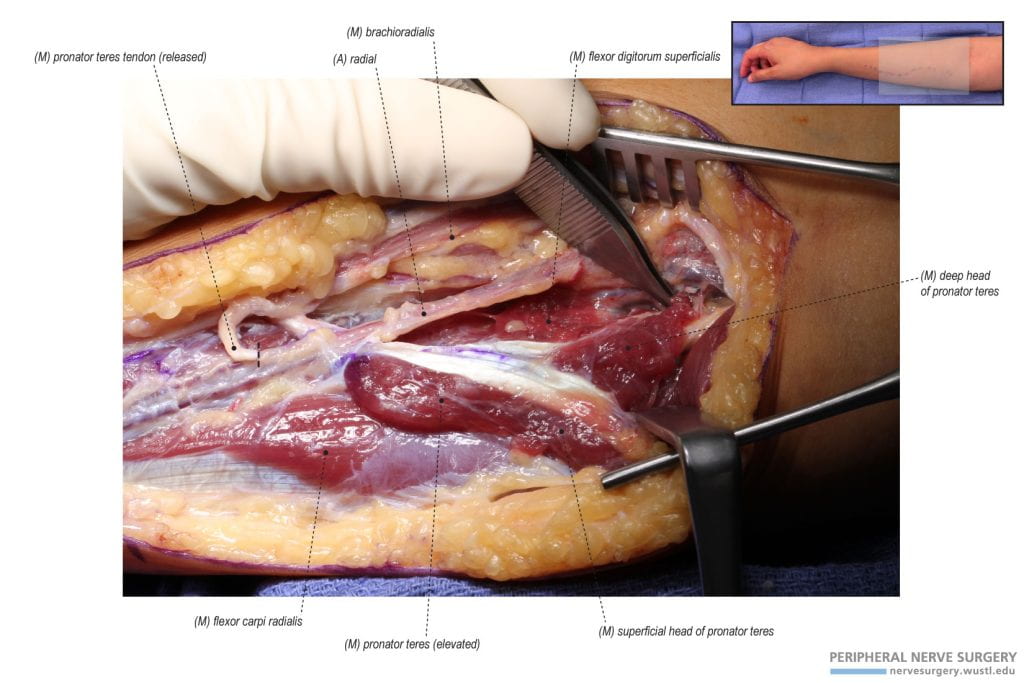
Figure 5 – Release of the pronator teres tendon from the radius for the pronator teres (PT) to extensor carpi radialis brevis (ECRB) tendon transfer. The pronator teres tendon is released from its insertion attachment to the radius and mobilized for the PT to ECRB tendon transfer. If this tendon transfer is not performed unlike in this case, the pronator teres remains attached and its tendon is step-lengthened.
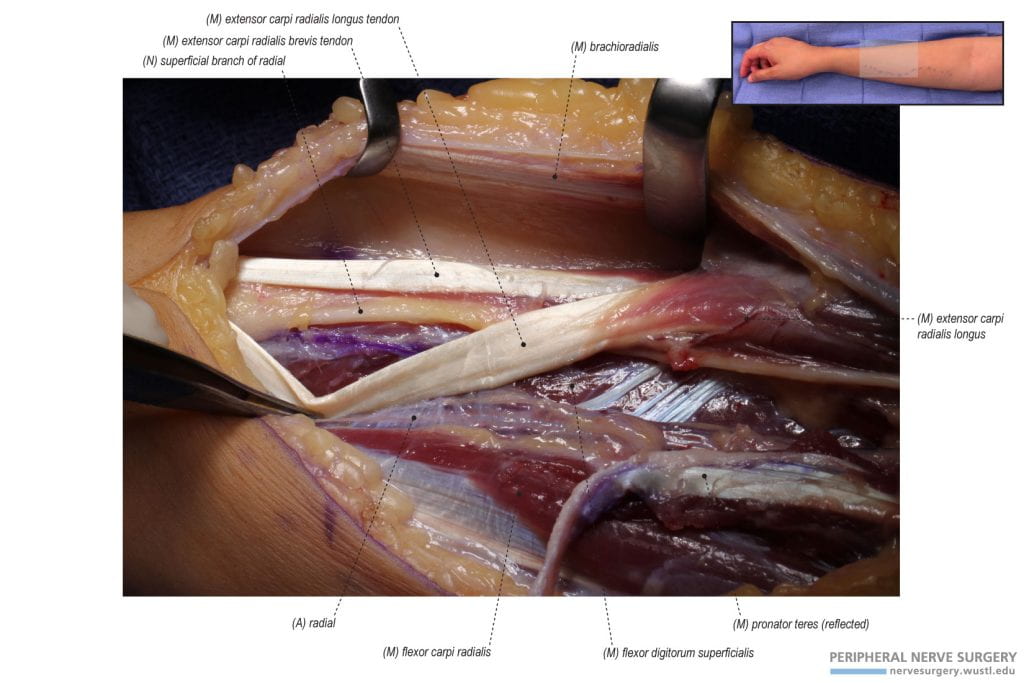
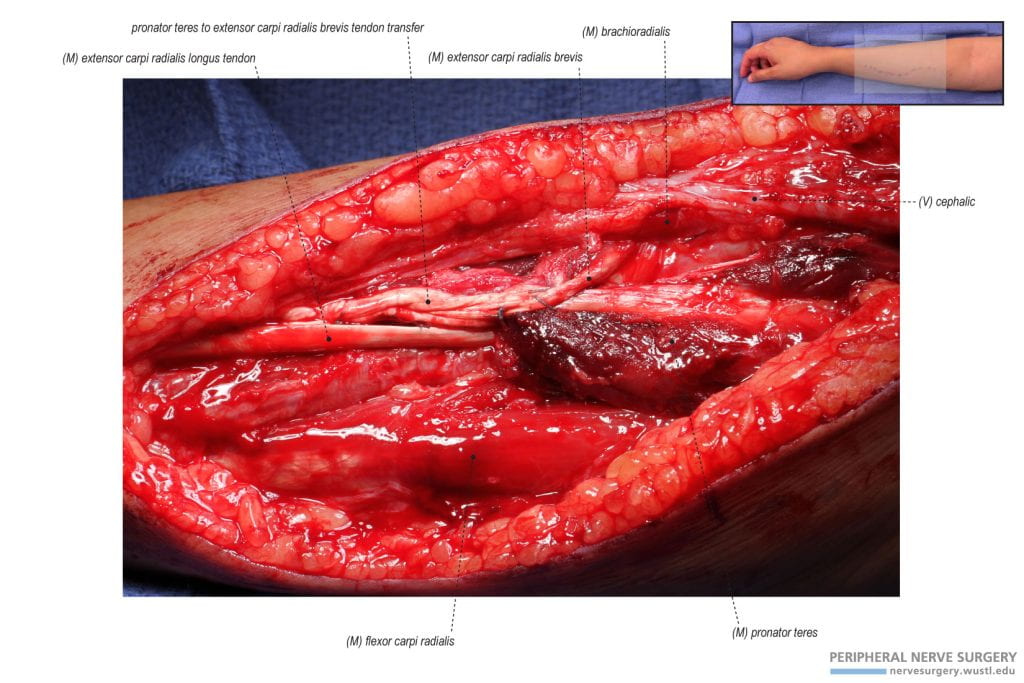
Figure 6 – Identifying extensor carpi radialis brevis (ECRB) inferior to extensor carpi radialis longus (ECRL). ECRB is located inferior to ECRL. Their function can be confirmed by pulling the respective tendon proximally and observing the actions of the hand. ECRL inserts at the dorsum of the first and second digits producing wrist extension with radial deviation, while ECRB inserts at the dorsum of the third digit producing specifically wrist extension.
Figure 7 – Identifying the recipient extensor carpi radialis brevis (ECRB) muscle for tendon transfer. The recipient ECRB for tendon transfer is located inferior to the extensor carpi radialis longus (ECRL). By retracting ECRL, the ECRB tendon is observed.
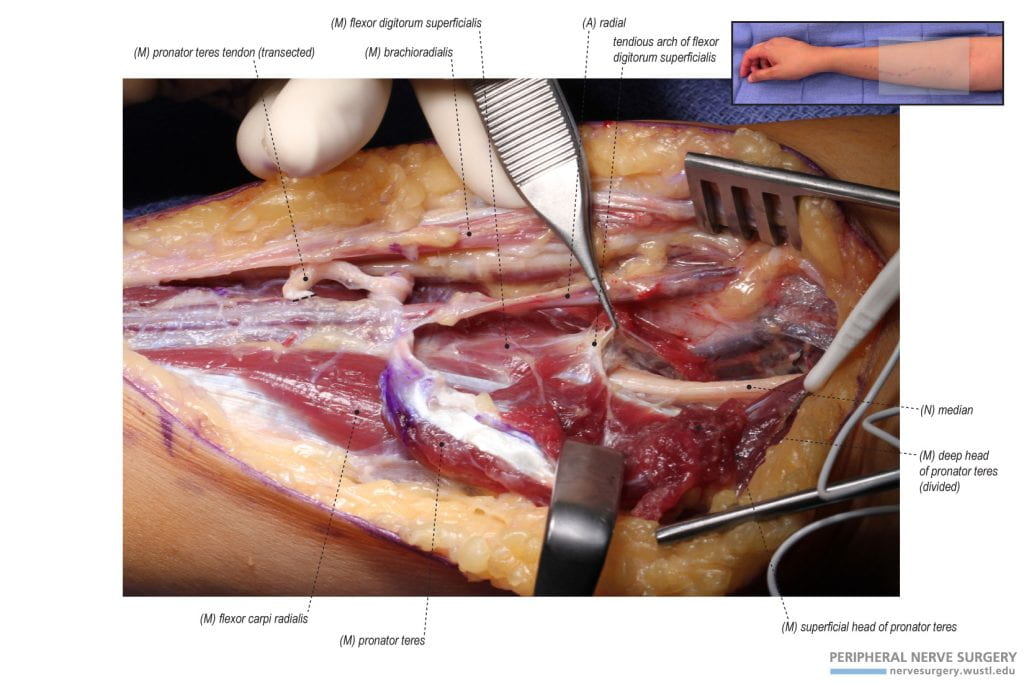
Figure 8 – Identifying the deep head of the pronator teres for the exposure of the median nerve. The deep head of the pronator teres is identified medial to the radial vessels and lateral to the superficial head. The deep head has a deep origin that superficial to the median nerve. The deep head of the pronator teres is divided to expose the median nerve.
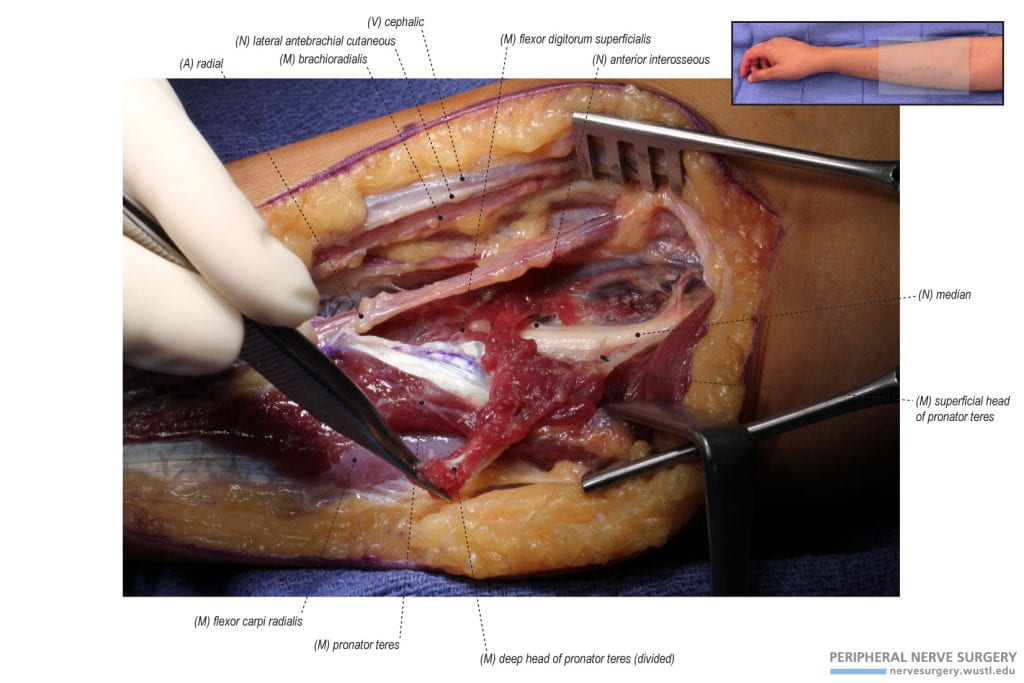
Figure 9 – Release of the deep head of the pronator teres. By releasing the deep head of the pronator teres, the median nerve is identified. The respective donor nerves for the median to radial nerve transfer are located on medial aspect of the median nerve. The anterior interosseous nerve can be used as a landmark to gauge where the donor nerves branches from the median nerve.
Figure 10 – Identifying and releasing the tendious arch of the flexor digitorum superficialis (FDS). The next structure that is released to further expose the median nerve is the tendious arch of the FDS. The tendious arch is seen with a sharp border and is responsible in some patients for median nerve compression at this level.
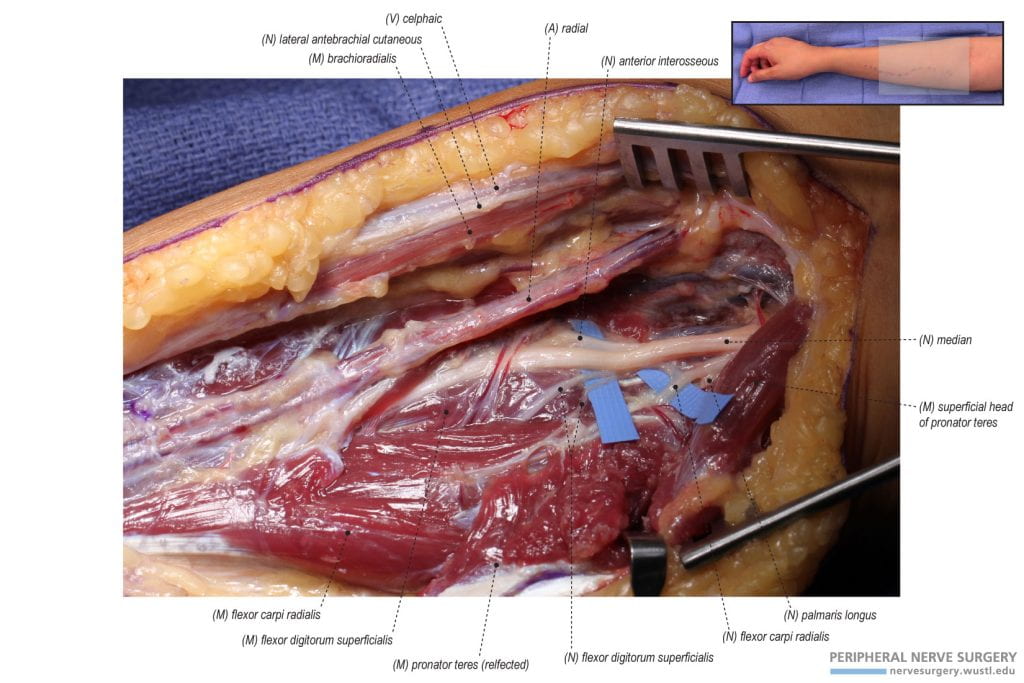
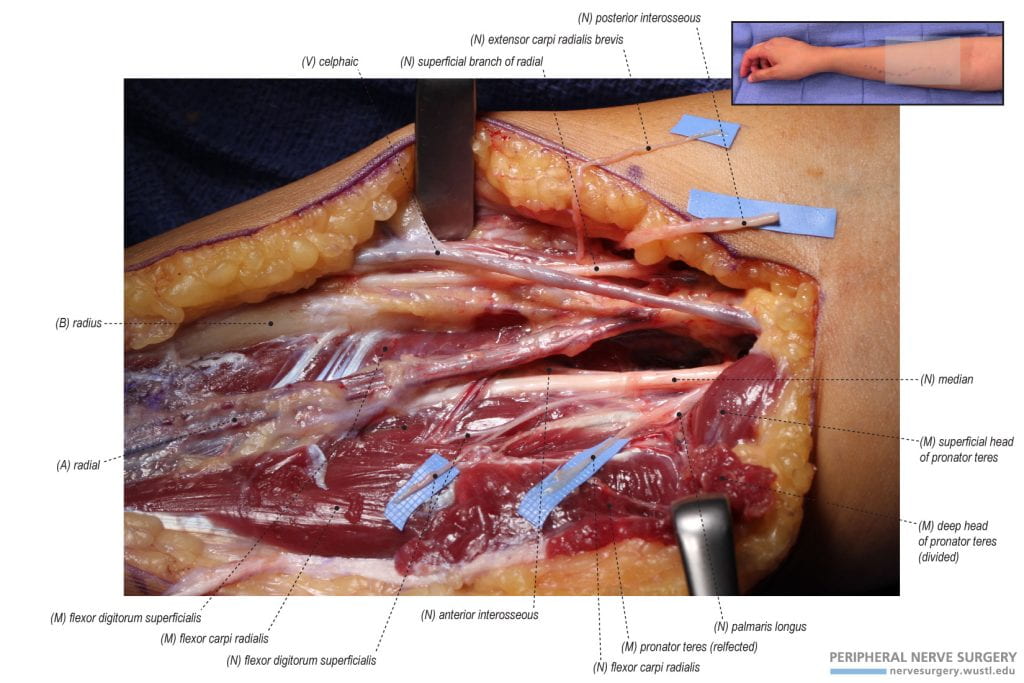
Figure 11 – Exposure of the median nerve and its donor branches. Following the release of the tendious arch of the flexor digitorum superficialis (FDS), the median nerve and its donor branches are identified. The donor flexor carpi radialis (FCR) nerve branch is identified proximally with the palmaris longus nerve branch. Distally, two donor FDS nerve branches are identified. In most cases, there is an additional FDS nerve branch distal to these branches. This can be confirmed by electrical stimulating the medial aspect of the median nerve.
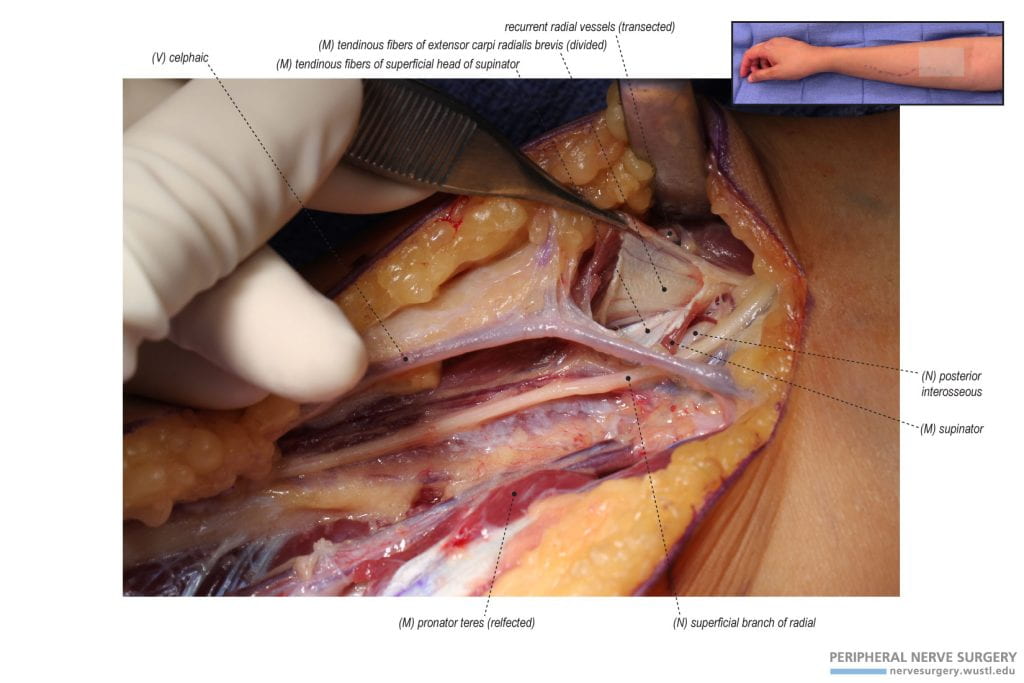
Figure 12 – Exposure of the radial nerve by dissecting through the tendinous fibers of the supinator. Moving to the lateral side of the radial vessels and retracting the brachioradialis, the superficial branch of the radial nerve is identified. Deep to this nerve are the recipients – posterior interosseous nerve (deep branch of the radial nerve) and the extensor carpi radialis brevis nerve branch. To expose these recipient nerves, requires dividing first the tendinous fibers of the extensor carpi radialis brevis and then the tendinous fibers of the superficial head of supinator.
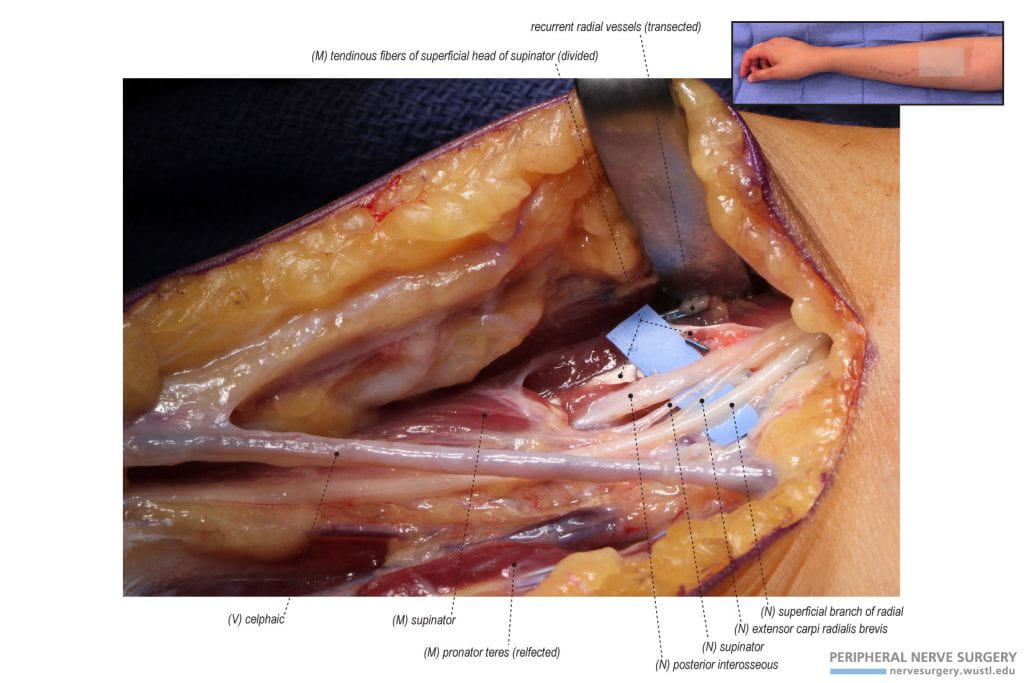
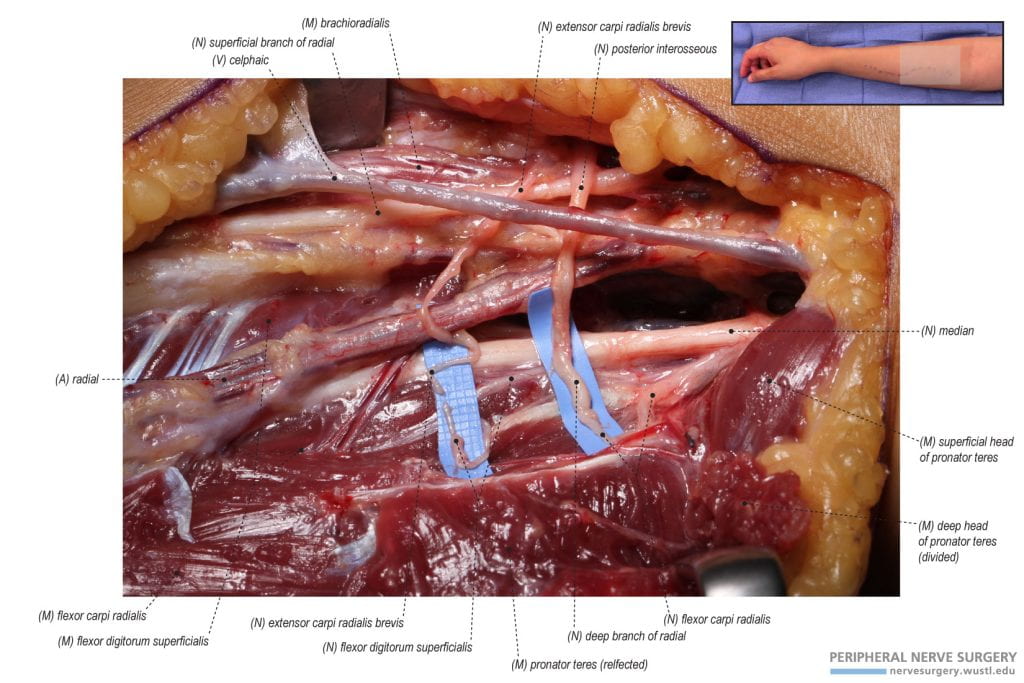
Figure 13 – Exposure of the radial nerve and its recipient branches. Following the release of the tendious fibers of the extensor carpi radialis brevis (ECRB) and supinator, the radial nerve and its recipient branches are exposed. Lateral to the superficial branch of the radial nerve is the recipient nerve to the ECRB. The posterior interosseous nerve (PIN) is the second recipient nerve and is identified lateral to the ECRB nerve. A supinator nerve is seen to branch from the medial and deep aspect of the PIN. The supinator nerve is not included in the median to radial nerve transfer.
Figure 14 – Donor median nerve and recipient radial nerve and its branches. The donor median nerve branches, flexor carpi radialis (FCR) and flexor digitorum superficialis (FDS), are observed. In addition, the recipient radial nerve branches, posterior interosseous nerve (PIN), and extensor carpi radialis brevis (ECRB), are observed. The supinator nerve is not included in the nerve transfer.
Figure 15 – Dividing the recipient posterior interosseous nerve (PIN) to not include the supinator nerve. The PIN is divided proximally with the supinator branch. The supinator branch is then neurolyzed from the PIN as it is included in the reconstruction. The supinator, being already deinnervated, is not a critical function designated for reinnervation.
Figure 16 – Transecting the donor median and recipient radial nerves for nerve transfer. To acquire sufficient length for nerve transfer, the donor median nerves, flexor carpi radialis (FCR) and flexor digitorum superficialis (FDS), are transected distally and the recipient radial nerves, posterior interosseous nerve (PIN) and extensor carpi radialis brevis (ECRB), are transected proximally.
Figure 17 – Median to radial nerve transfer. The median to radial nerve transfer is composed of two transfers. (1) The donor flexor carpi radialis (FCR) nerve is transferred to the recipient posterior interosseous nerve (PIN). (2) The donor flexor digitorum superficialis (FDS) nerve is transferred to the recipient extensor carpi radialis brevis (ECRB) nerve.
Figure 18 – Weaving the donor pronator teres tendon into the recipient extensor carpi radialis brevis (ECRB) tendon. After identifying the ECRB tendon, a weaving forceps is used to pierce the ECRB tendon to grasp the pronator teres tendon. This first weave sets the tension for the tendon transfer.
Figure 19 – Pronator teres to extensor carpi radialis brevis (ECRB) tendon transfer. Following the first weave and the tension is set, the pronator teres and ECRB tendons are sutured several times together. Following, the ECRB tendon is woven several times distally into the pronator teres tendon and sutured together.