Key Points:
- Assess both extrinsic and intrinsic median innervated muscles; check for anterior interosseous nerve branch versus median nerve proper function.
- Extrinsic muscles provide pronation, wrist flexion, thumb interphalangeal joint flexion, finger proximal interphalangeal joint flexion and index +/- long finger distal interphalangeal joint flexion. Exam of palmaris longus is important when performing tendon transfer surgery where it can be used as a donor tendon.
- Intrinsic muscles provide thumb palmar abduction and opposition; and index and long finger lumbrical function.
- The anterior interosseous branch of the median nerve specifically provides innervations for thumb interphlangeal joint flexion, index finger distal interphalangeal joint flexion and pronation via pronator quadratus.
- Extrinsic muscles provide pronation, wrist flexion, thumb interphalangeal joint flexion, finger proximal interphalangeal joint flexion and index +/- long finger distal interphalangeal joint flexion. Exam of palmaris longus is important when performing tendon transfer surgery where it can be used as a donor tendon.
- Sensory examination includes testing the median-specific digital cutaneous nerves (palmar aspect of the thumb, index, long and radial half of ring finger) and palmar median cutaneous nerve territory.
- Originates from roots: C6-T1.
EXAMINATION
- Physical examination of the median nerve includes both motor and sensory examination.
- Median nerve function is particularly important in that it contributes to the following median-nerve-only innervated motor functions: forearm pronation, thumb palmar abduction, and thumb/index/long finger flexion. It is also provides sensation to critical areas of the hand—the pinch surfaces of the thumb and index fingers. The median nerve also contributes to pinch and grip strength.
Detailed Examination Links:
Proximal Extrinsic Motor Branches (Median Nerve)
- Pronator teres
- Flexor carpi radialis
- Flexor digitorum superficialis
- Palmaris longus
- Triceps brachii / Anconeus
Proximal Extrinsic Motor Branches (Anterior Interosseous Nerve)
- Flexor pollicis longus
- Flexor digitorum profundus (to index and, usually, long finger)
- Pronator quadratus.
Distal Intrinsic Motor Branches (Thenar Branch)
- Abductor pollicis brevis
- Flexor pollicis brevis (superficial head)
- Opponens pollicis
Distal Intrinsic Motor Branches (Common Digital Branches of the Median Nerve)
- 1st and 2nd lumbrical (to index and long fingers)
Sensory Branches
- Common and proper digital nerves (to volar thumb, index, long, and radial half of ring finger)
- Palmar branch (to radial base of palm)
- Articular branches to the elbow and wrist joints (via distal anterior interosseous nerve)
Summarized Examination:
- Forearm pronation—place the patient’s forearm in the pronated position and ask the patient to maintain that position; attempt to rotate the forearm into supination (tests pronator teres and quadratus).
- Wrist flexion—palpate the flexor carpi radialis and (with the thumb and small finger in opposed and wrist flexed) the palmaris longus.
- Finger flexion—ask the patient to flex at the proximal interphalangeal joint of each finger individually and at the distal interphalangeal joint of the index and long fingers (tests flexor digitorum superficialis, and median-innervated flexor digitorum profundus).
- Finger metacarpal phalangeal joint flexion and interphalangeal joint extension of the index and long fingers (tests for median-innervated lumbrical function).
- Thumb movement—ask the patient to flex the interphalangeal joint of the thumb (to assess flexor pollicis longus). Also, ask the patient to perform palmar abduction of the thumb and opposition.
- Sensation to the volar thumb and index finger.
Pathological Findings:
Known sites of median nerve compression or entrapment:
- Axilla: at anomalous vascular perforators or arcades that tether or compress the nerve.
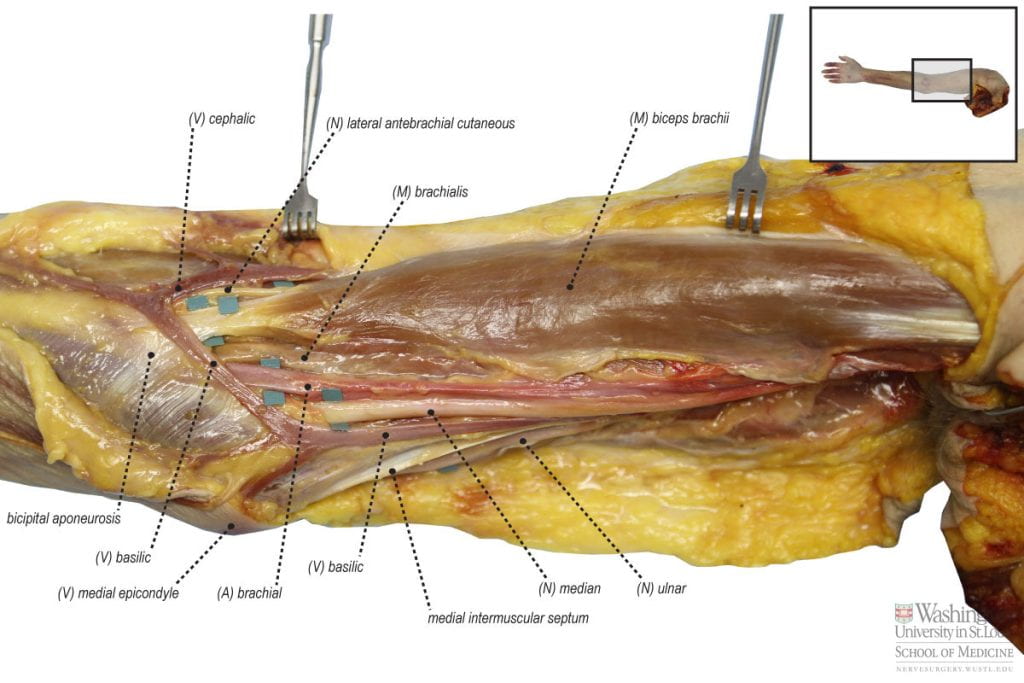
- Brachium:
- At the supracondylar process or Struther’s ligament (this is a bony process that arises from the humerus just proximal to the elbow)–increasingly rare (disappearing d/t evolutionary changes).
- At the lacertus fibrosis (thick fibers that compress the nerve at the level of the antecubital fossa) this can be a site of compression especially after localized bleeding in the area due to vascular puncture or spontaneous bleeding seen with hypocoagulable states.
- At crossing vessels in the antecubital region.
- At the supracondylar process or Struther’s ligament (this is a bony process that arises from the humerus just proximal to the elbow)–increasingly rare (disappearing d/t evolutionary changes).
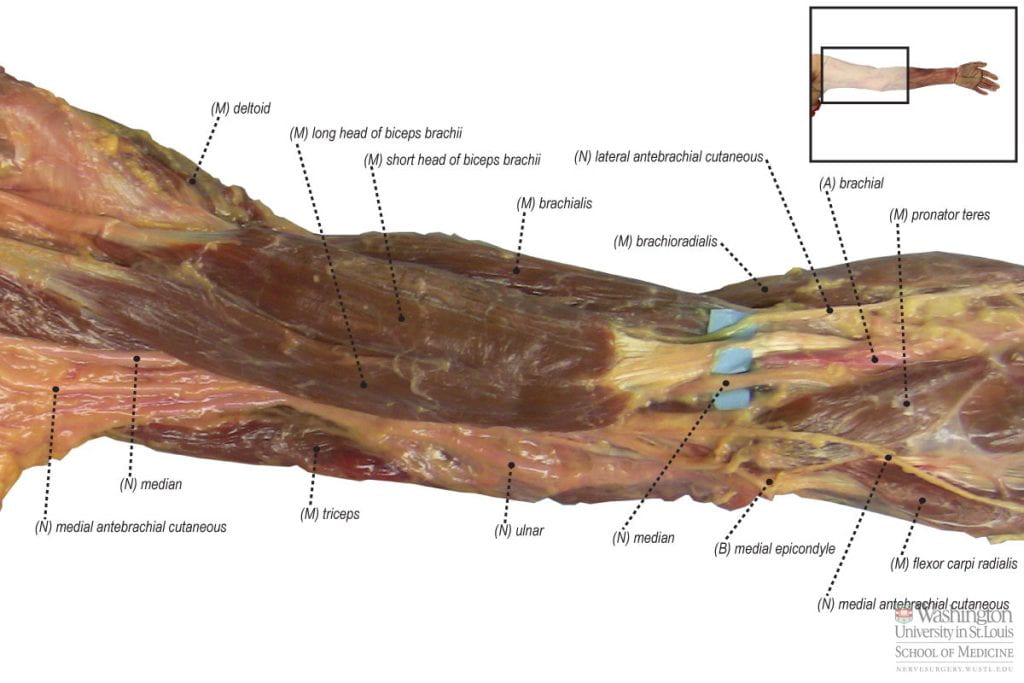
- Proximal Forearm/Elbow:
- Due to anomalous ligaments and/or large underlying brachialis muscle at the antecubital fossa
- At the pronator teres origin–the deep and superficial head fibrous arches of this muscle can compress either the median nerve proper and/or the anterior interosseous nerve.
- At the flexor digitorum superficialis muscle origin fibrous arch.
- At the following anomalous muscles:
- Gantzer’s muscle, which is an accessory slip of the flexor pollicis longus muscle.
- At a palmaris profundus anomalous muscle.
- At a flexor carpi radialis brevis anomalous muscle.
- Gantzer’s muscle, which is an accessory slip of the flexor pollicis longus muscle.
- Due to anomalous ligaments and/or large underlying brachialis muscle at the antecubital fossa
- Wrist/Hand: Commonly known as carpal tunnel syndrome (compression of the median nerve at the transverse carpal ligament at the wrist/proximal hand).
Specific Named Compressive/Entrapment Syndromes:
- Pronator Teres Syndrome: see above
- Patients complain of aching in forearm, especially with pronation of forearm activities
- Provocative testing in the proximal arm may be positive (Tinel’s, scratch-collapse).
- Reproduction of pain with resisted passive supination.
- Numbness, tingling, distal motor weakness may also be seen (at prontaor teres, flexor digitorum, thenar musculature).
- Anterior Interosseous Nerve Syndrome: see above
- Isolated motor symptoms: loss of flexor pollicis longus and index (+/- long) finger flexor digitorum profundus function.
- Patients have loss of ability to make the “OK” sign as they can not flex the thumb at the interphalangeal joint and index finger at the distal interphalangeal joint.
Clinical Relevance:
- The median nerve is critical to normal upper extremity function (but remains second to ulnar nerve in terms of the critical function provided to the hand).
- Isolated median nerve injury is most debilitating for the loss of forearm pronation, loss of sensation at the pinch surfaces of the thumb and index finger; as well as the loss of index +/- long finger flexion and thumb function.
- In median nerve injury patterns, when the denervation time permits (3 to 6 months or less is ideal), restoration of pronation is critical and can be accomplished through radial to median nerve transfer procedures (for example the extensor carpi radialis brevis nerve branch may be transferred to the pronator teres nerve branch). Radial to median nerve transfer can also be used to restore thumb and index finger flexion. In chronic injuries, tendon transfers can restore finger and thumb median-innervated function but options are poor to restore pronation. Nerve transfer to restore the vital sensation to the first webspace can be restored irrespective of time since injury since sensory nerve injuries are not time sensitive.
- Restoration of median innervated loss of function associated with lower or complete brachial plexus injury is challenging indeed and the ability to restore complete normal hand function remains elusive in adults.
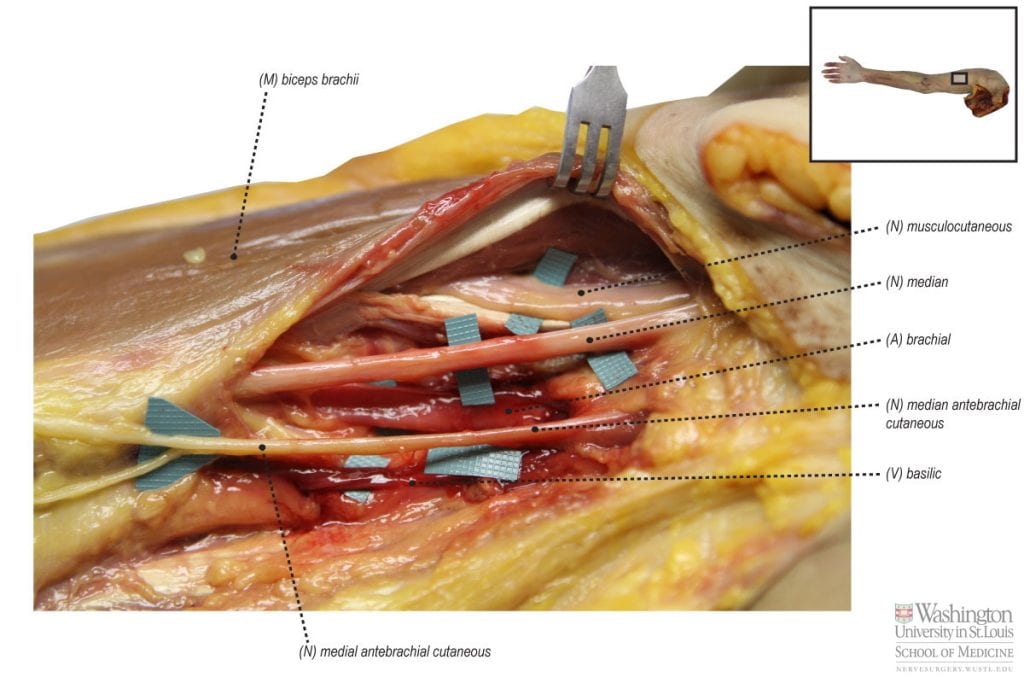
- Direct median nerve injury in the arm is often due to penetrating injury, and commonly associated with injury to the brachial artery as these two structures travel close together.
- The median nerve is commonly noted for its susceptibility to compression neuropathy, particularly at the carpal tunnel. Examination of compressive neuropathy includes all of the above mentioned techniques to examine motor and sensory dysfunction as well as the performance of provocative maneuvers at known sites of compression (see above).
Relevant Anatomy
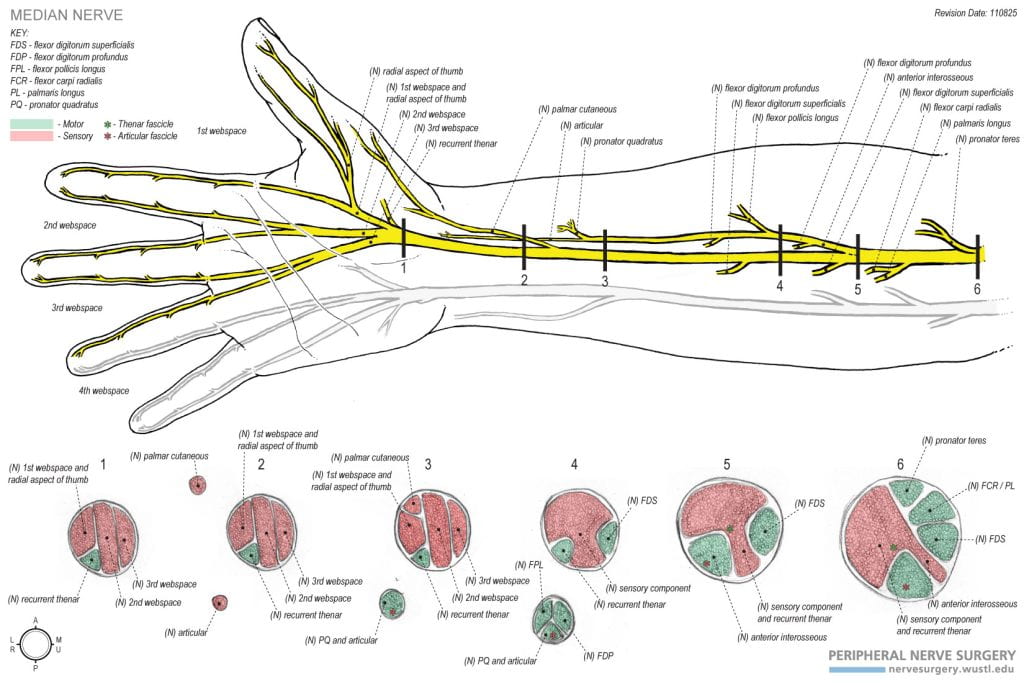
Innervation:
- Roots: C6-T1.
- Nerve: Median nerve.
- Muscles Innervated: Pronator teres, flexor carpi radialis, flexor digitorum superficialis, palmaris longus, flexor pollicis longus, flexor digitorum profundus (radial ½), pronator quadratus, abductor pollicis longus, flexor pollicis (superficial head), opponens pollicis. 1st and 2nd lumbricals.
- Sensory Distribution Innervated: Common and proper digital nerves, palmar branch, and articular branches to the elbow and wrist joints.
- Innervation Route:
- Muscles
- C6, C7 → median nerve → pronator teres branch.
- C6, C7 → median nerve → flexor carpi radialis branch.
- C7, C8 → median nerve → flexor carpi radialis and palmaris longus branch → palmaris longus branch.
- C7, C8, T1 → median nerve → flexor digitorum superficialis branches.
- C7, C8, T1 → median nerve → flexor pollicis longus branch.
- C8, T1 → median nerve → anterior interosseous nerve → flexor digitorum profundus I, II branches.
- C8, T1 → median nerve → anterior interosseous nerve → pronator quadratus branch.
- C8, T1 → median nerve → thenar branch → abductor pollicis brevis branch.
- C8, T1 → median nerve → thenar branch → flexor pollicis brevis (superficial head).
- C8, T1 → median nerve → thenar branch → Opponens pollicis.
- C8, T1 → median nerve → proper palmar digital nerve → lumbrical I branch.
- C8, T1 → median nerve → common palmar digital nerve → lumbrical II branch.
- Sensation
- C6, C7 → median nerve → palmar cutaneous branch of median nerve.
- C6, C7, C8 → median nerve → digital cutaneous branches of median nerve.
- Muscles