Title: Thoracic Outlet Decompression.
Published: 5/17/2011, Updated: 5/17/2011.
Author(s): Susan E. Mackinnon MD, Andrew Yee BS, Osvaldo Laurido-Soto BS.
Division of Plastic and Reconstructive Surgery, Washington University School of Medicine, St. Louis, MO.
Thoracic outlet syndrome (TOS) is controversial and difficult to diagnose due to the wide-range of symptomology (vascular and/or neurogenic) that are involved, may it be vascular and/or neurogenic, and there not being a distinct examination method (1). The superior thoracic outlet, anatomically known as the thoracic inlet, is composed of the anterior and middle scalene between which the brachial plexus, subclavian artery, and subclavian vein courses distal, superior to the 1st rib and passes obliquely and inferiorly to the clavicle. Impingement of the brachial plexus can involve these structures. As there can be a neurogenic, arterial, and/or venous component of TOS, the most common is neurogenic and constitute the majority of patients with complaints of diffuse shoulder weakness, postural abnormalities, and pain/numbness in the affected upper extremity. Non-invasive treatment for TOS can involve posture correction, shoulder muscles strengthening, and stretching to promote nerve gliding and relieve pressure off of the brachial plexus through the thoracic outlet. Therefore, diagnosis of TOS is made frequently; rarely do these patients require surgical decompression (1). If conservation management fails, our institution’s preferred approach for decompression of the brachial plexus for neurogenic TOS is a supraclavicular approach to release the scalene muscles. Initially, the procedure included a first rib resection, but over the last two decades, literature has shown that the release of the scalene muscles is as satisfactory in results as with the first rib resection. Resection of the first rib is not necessary, unless there is a vascular component to the thoracic outlet syndrome or an underlining pathology in the bony structures. Decompression of the brachial plexus for neurogenic TOS primarily involves dividing the anterior and middle scalene muscles and inspecting the brachial plexus and its nerve branches for possible compression points by adjacent structures.
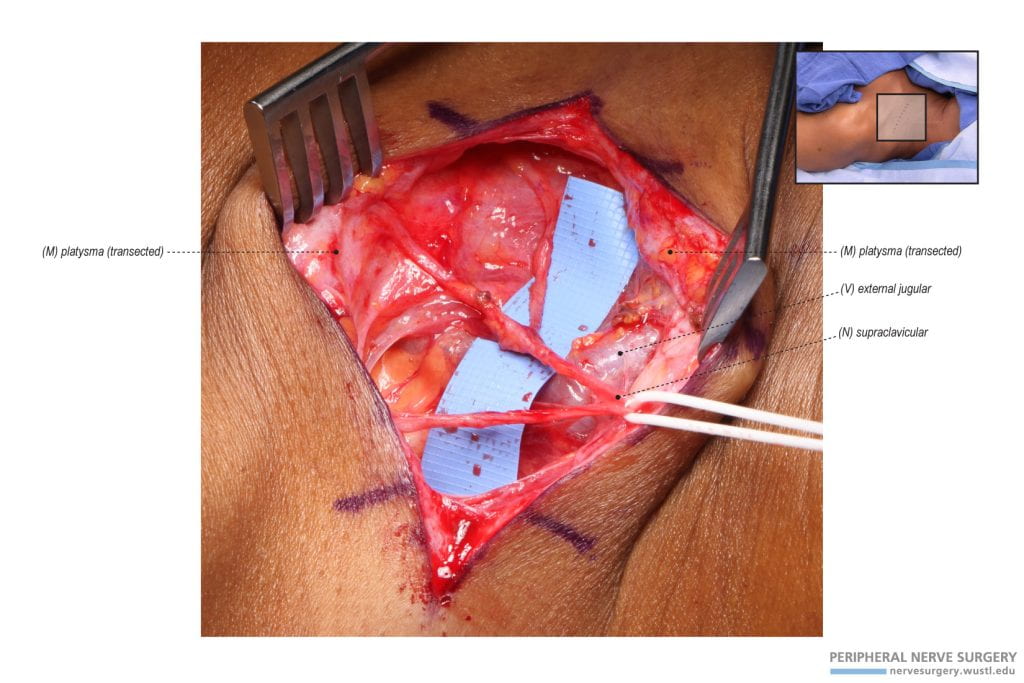
Figure 1 – Supraclavicular Incision for a Thoracic Outlet Decompression. An incision is made a finger breath supraclavicular and approximately 8cm in length. The arm tourniquet depicted in this figure was unique to this case and not for the thoracic outlet decompression, but specific for an ulnar nerve transposition at the cubital tunnel.
Figure 2 – Exposure and Identification of the Supraclavicular Nerves. Upon exposure, the platysma is initially identified and divided. Beneath the platysma, the supraclavicular nerve and its branches are identified, carefully dissected both proximally and distally, and protected. The supraclavicular nerve branches originate from a proximal trunk noted with a vessel loop. Two vessel loops are used to protect and retract the supraclavicular nerves. In this specific case, the platysma was scarce.
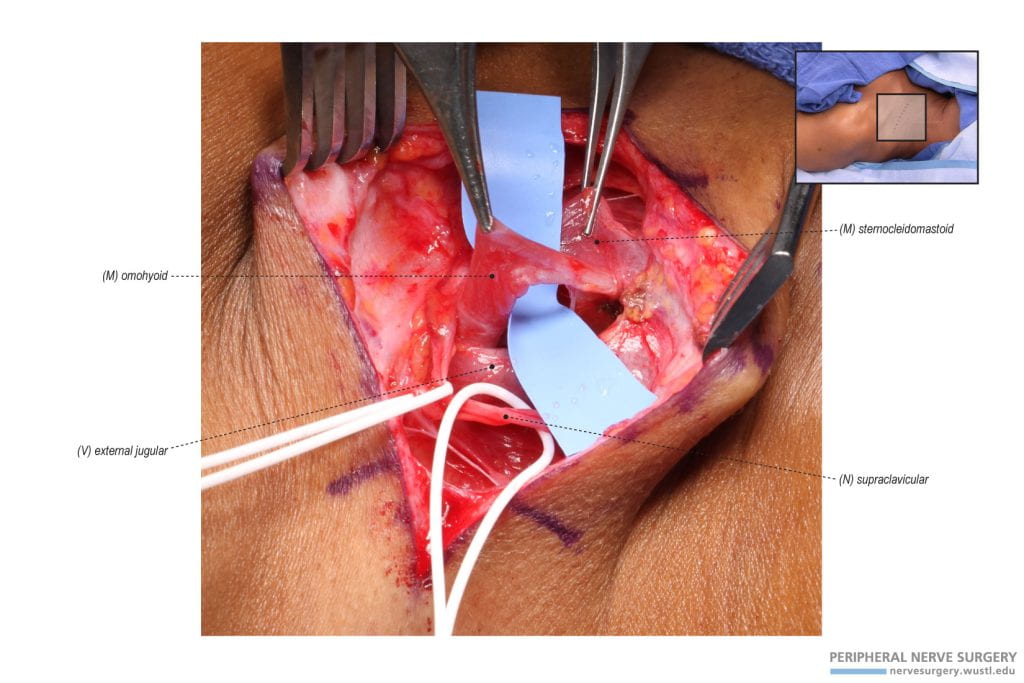
Figure 3 – Exposure and Identification of the Omohyoid. The sternocleidomastoid and external jugular vein are identified upon further exposure and the dissection continues on a plane beneath the sternocleidomastoid. The omohyoid is identified through this plane and divided to expose the anterior scalene and brachial plexus. The supraclavicular nerve is protected and mobilized by two vessel loops.
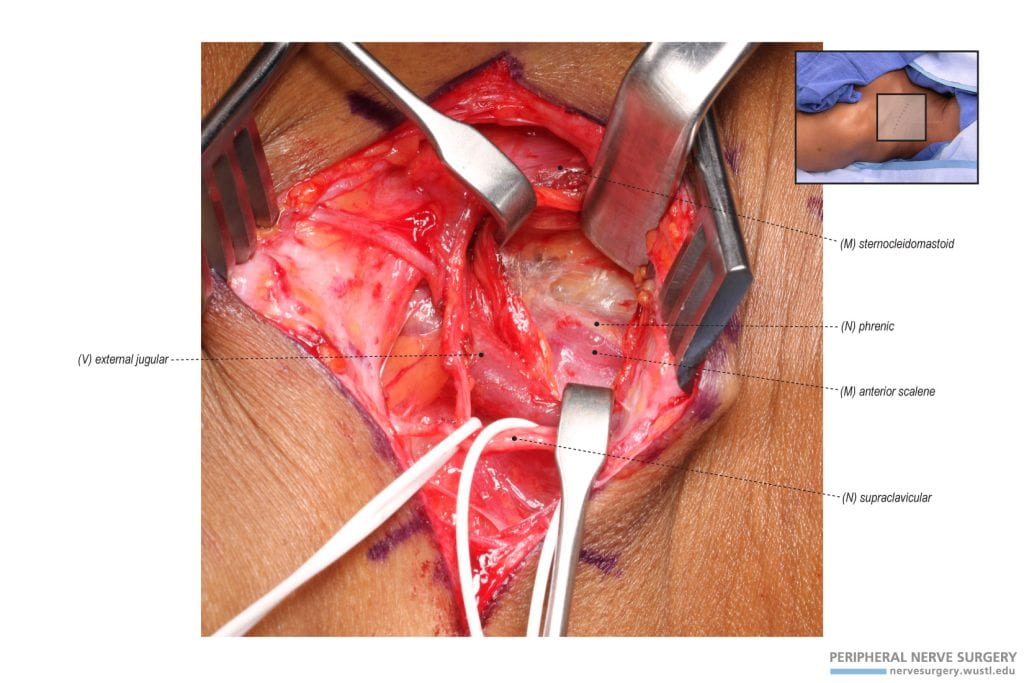
Figure 4 – Exposure and Identification of the Anterior Scalene and Phrenic Nerve. Upon dividing the omohyoid and further dissection, the phrenic nerve is identified on the anterior surface of the anterior scalene. The nerve has a lateral to medial course to innervate the diaphragm. The phrenic nerve is isolated and protected by gentle retraction. Due to the sensitivity and critical function of this nerve, a vessel loop is not used to protect the nerve. The anterior scalene is identified deep to this nerve and occasionally an accessory phrenic nerve is present and has a course through this muscle.
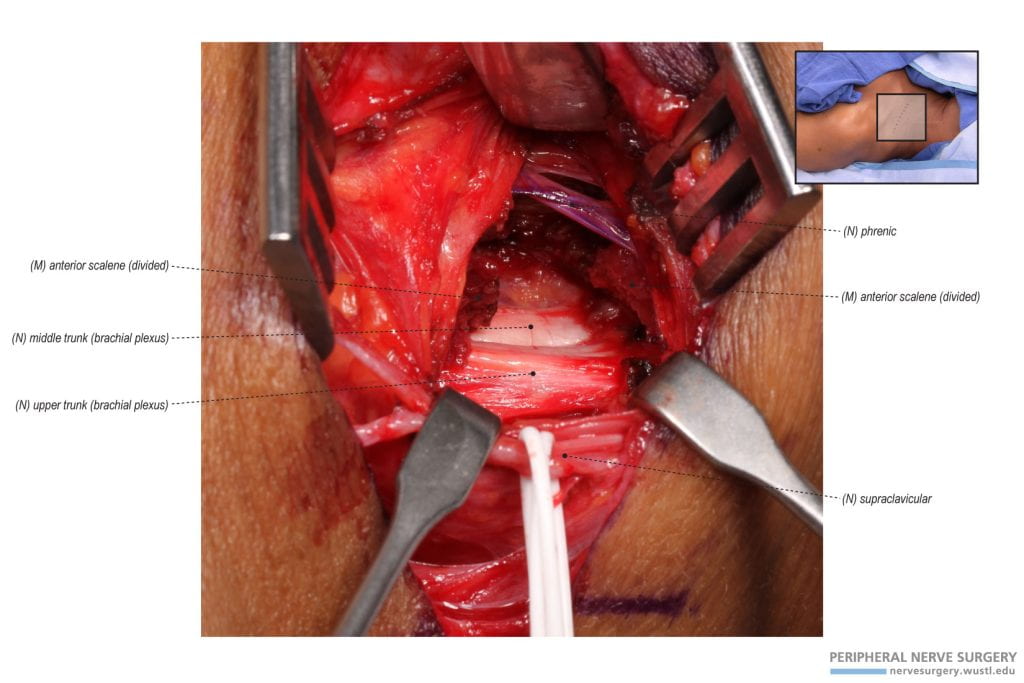
Figure 5 – Decompressing the Brachial Plexus by Dividing the Anterior Scalene. The anterior scalene is divided with the phrenic nerve noted and protected by gentle retraction. Occasionally, an accessory phrenic nerve is present and has a course through the anterior scalene. If encountered during the division of the anterior scalene, it is protected. The phrenic nerve has been marked in purple for visualization. The upper and middle trunks are visualized following the division of the anterior scalene.
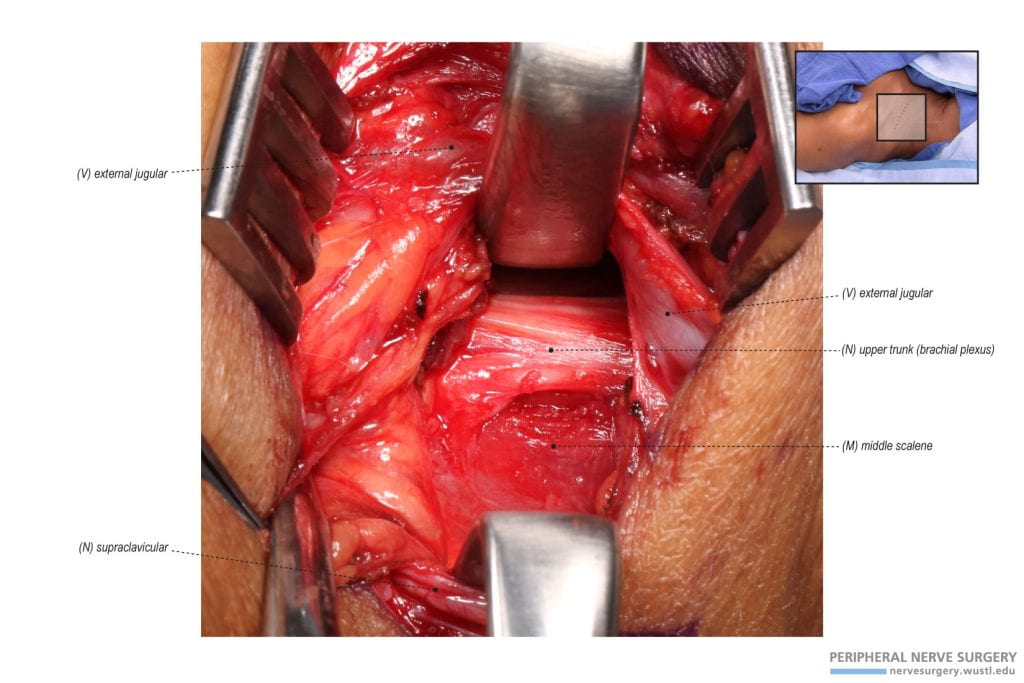
Figure 6 – Exposure and Identification of the Middle Scalene. To identify and divide the middle scalene, the surgical approach continues lateral to the brachial plexus. The middle scalene is identified lateral to the brachialis plexus. Typically, the long thoracic nerve has a course through this muscle or posterior to it. In this case, the long thoracic nerve was identified deep and lateral to the middle scalene.
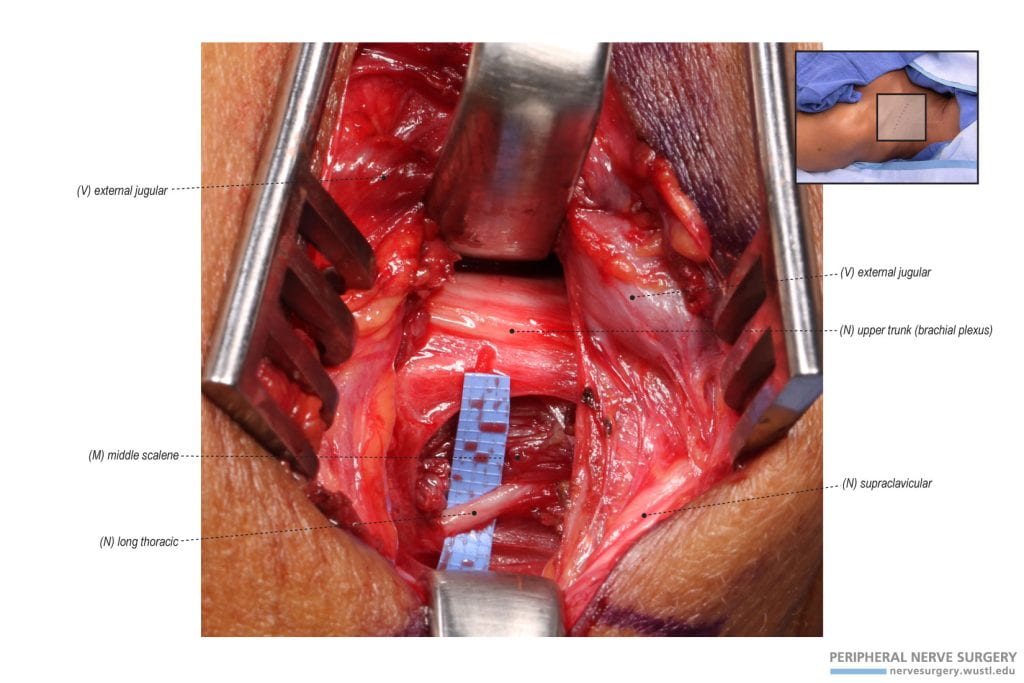
Figure 7 – Identification of the Long Thoracic Nerve. In this case, the middle scalene was briefly divided to identify the long thoracic nerve. The long thoracic nerve had a course through the middle scalene and deep and lateral to the middle scalene. This nerve is isolated and protected. A vessel loop can be used, unlike the phrenic nerve.
Figure 8 – Decompressing the Brachial Plexus by Dividing the Middle Scalene. The brachial plexus is further decompressed by dividing the middle scalene on its lateral side. A tendinous band of the middle scalene was identified deep in this case and was released in this case. The lower trunk is identified following the division of the middle scalene. The long thoracic nerve is protected by retraction.
Figure 9 – Thoracic Outlet Decompression and Relevant Anatomy. Following the division of the anterior and middle scalene to decompress the brachial plexus, the anatomical structures are reviewed for their integrity. The phrenic nerve is identified having a lateral to medial course to innervate the diaphragm. The long thoracic nerve is identified to innervate the serratus anterior. The supraclavicular nerves are protected by vessel loops. The upper, middle, lower trunks are reviewed to be intact and decompressed. Electrical stimulation is used to test motor nerve response.