Procedures – Tibial Nerve
Lower Leg
Title: Tibial Nerve Decompression at the Soleus.
Published: 3/28/2011, Updated: 3/28/2011.
Author(s): Susan E. Mackinnon MD, Andrew Yee BS.
Division of Plastic and Reconstructive Surgery, Washington University School of Medicine, St. Louis, MO.
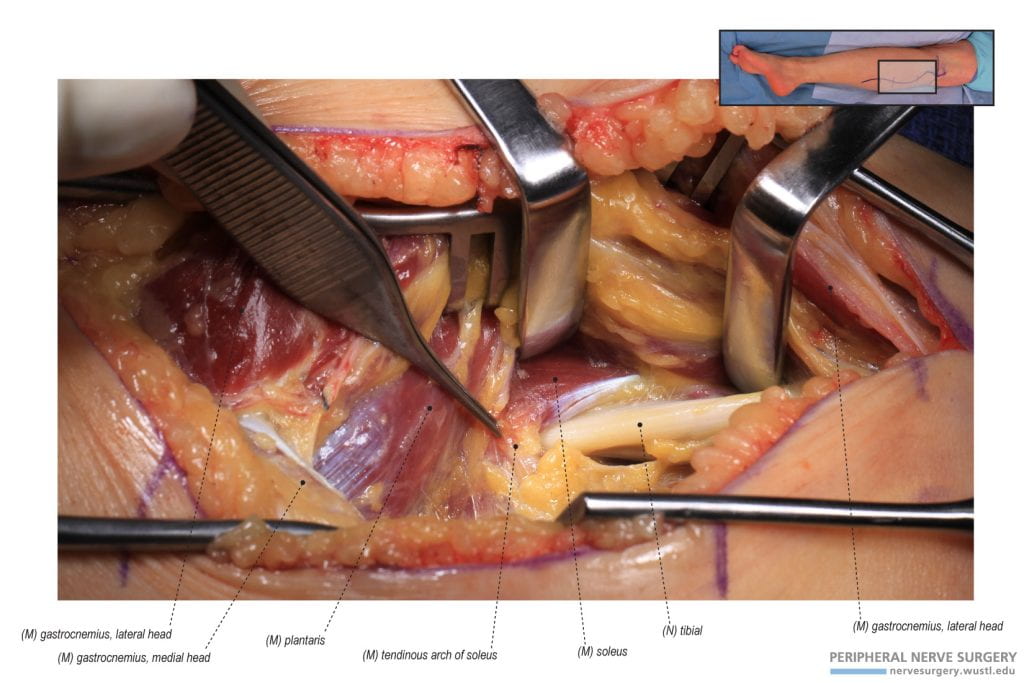
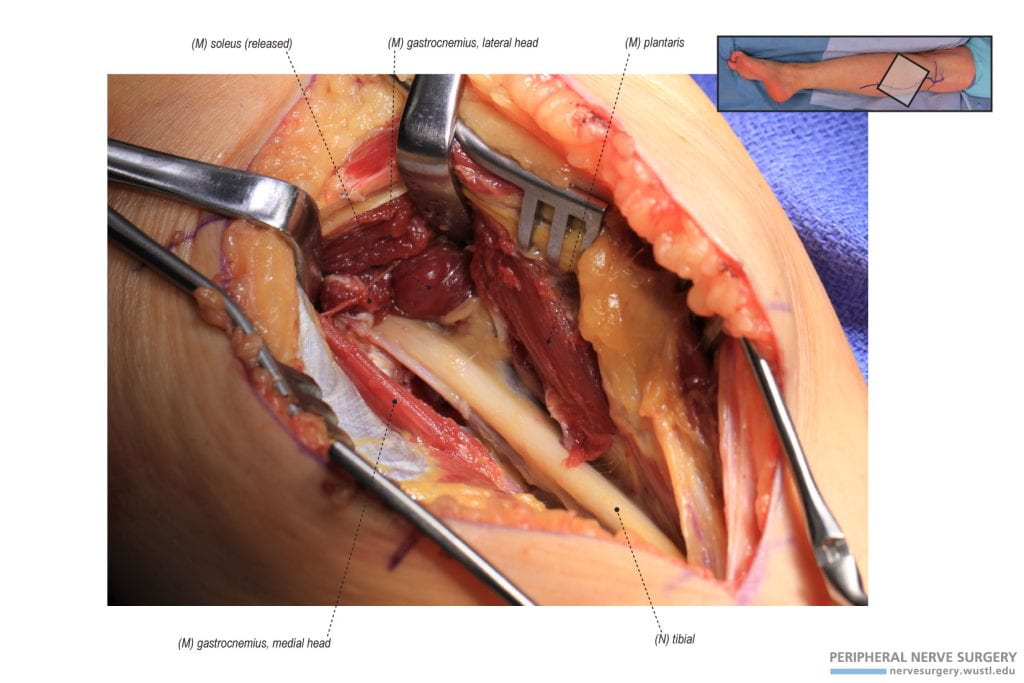
Figure 1 – Identifying the Tibial Nerve in the Lower Leg. The tibial nerve is identified by dissecting between and retracting the lateral and medial heads of gastrocnemius in the posterior and superior aspect of the lower leg. The tibial nerve courses deep to the soleus and its tendinous arch.
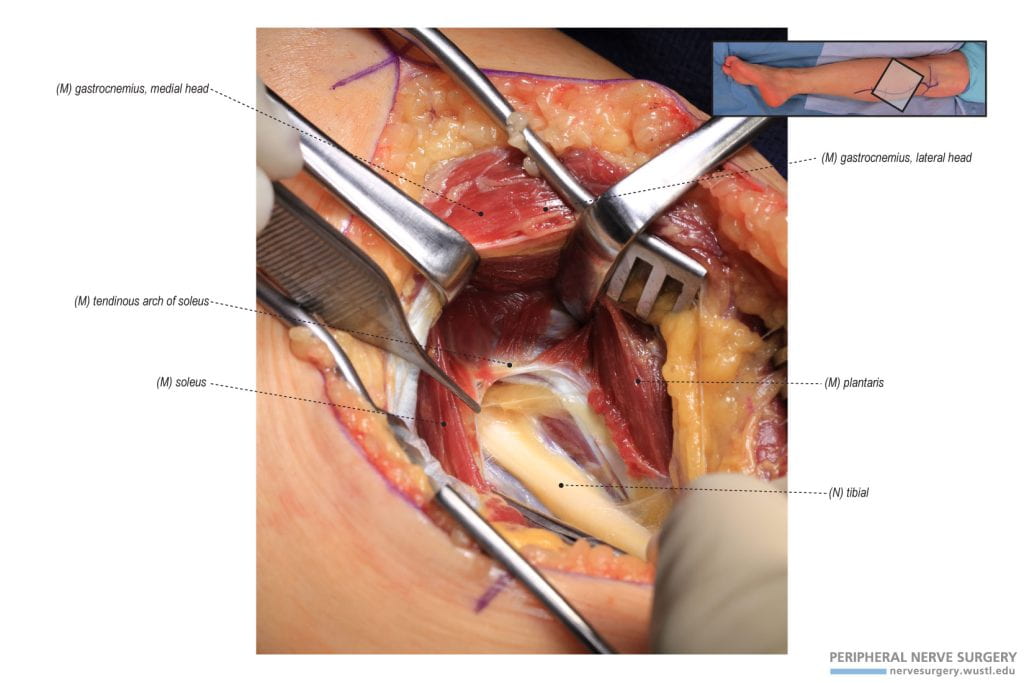
Figure 2 – Identifying the Tendinous Arch of Soleus. Further dissection, between the retracted lateral and medial heads of the gastrocnemius, reveals the tendinous arch of soleus. The appearance of the tendinous arch describes its compressive nature with the sharp arch.
Figure 3 – Decompression of the Tibial Neve at the Soleus. Decompression of the tibial nerve at the soleus occurs by releasing the tendinous arch of the soleus and performing a step-lengthening/tenotomy on the soleus tendon that is found compressing the tibial nerve.
Foot
Title: Tarsal Tunnel Release
Published: 10/13/2011, Updated: 10/13/2011.
Author(s): Andrew Yee BS, Susan E. Mackinnon MD.
Division of Plastic and Reconstructive Surgery, Washington University School of Medicine, St. Louis, MO.
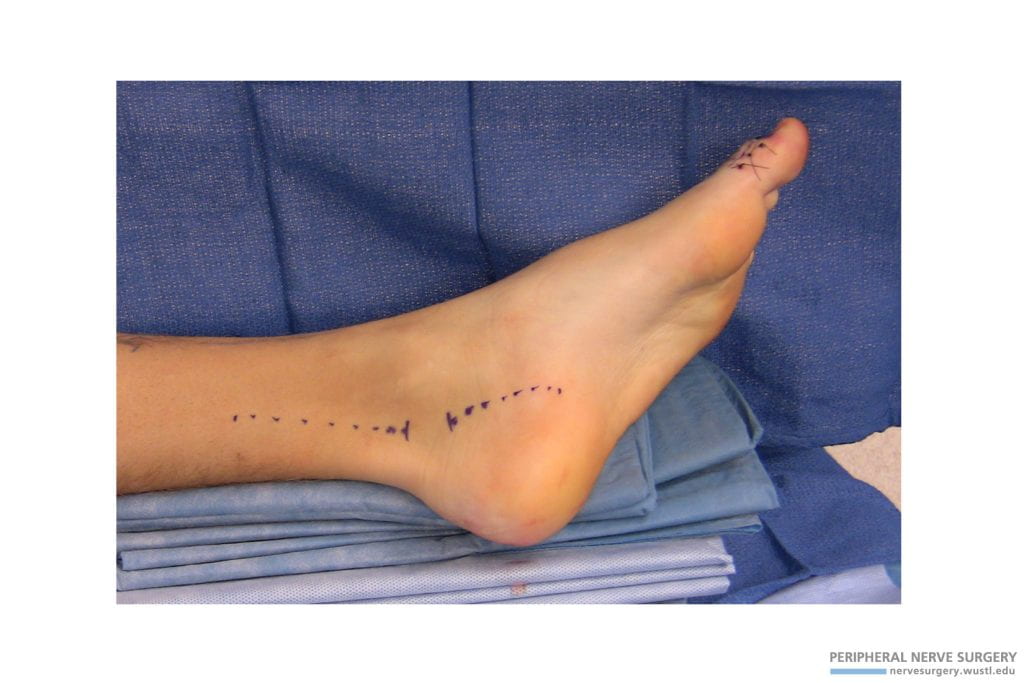
Figure 1 – Incision and positioning. Our approach for the tarsal tunnel release involves two incisions. The first incision is on the posterior third of the medial aspect of the lower leg over the course of the tibial nerve. The second incision is at an angle on the foot over the course of the lateral planter branch of tibial nerve. In our experience, the two linear incisions help promote healing following the release by leaving an intact short skin bridge.
Figure 2 – X-ray of the left foot following a traumatic injury and tibial nerve injury. In this specific case, this patient, following traumatic injury, had pain and numbness in the tibial nerve distribution along with Tinel’s sign and a positive scratch collapse at the tarsal tunnel. The scar tissue seen in the following case images during exposure are due to the traumatic injury and open reduction and internal fixation. A plate is seen on the tibia and a hammer toe reconstruction was performed simultaneously.
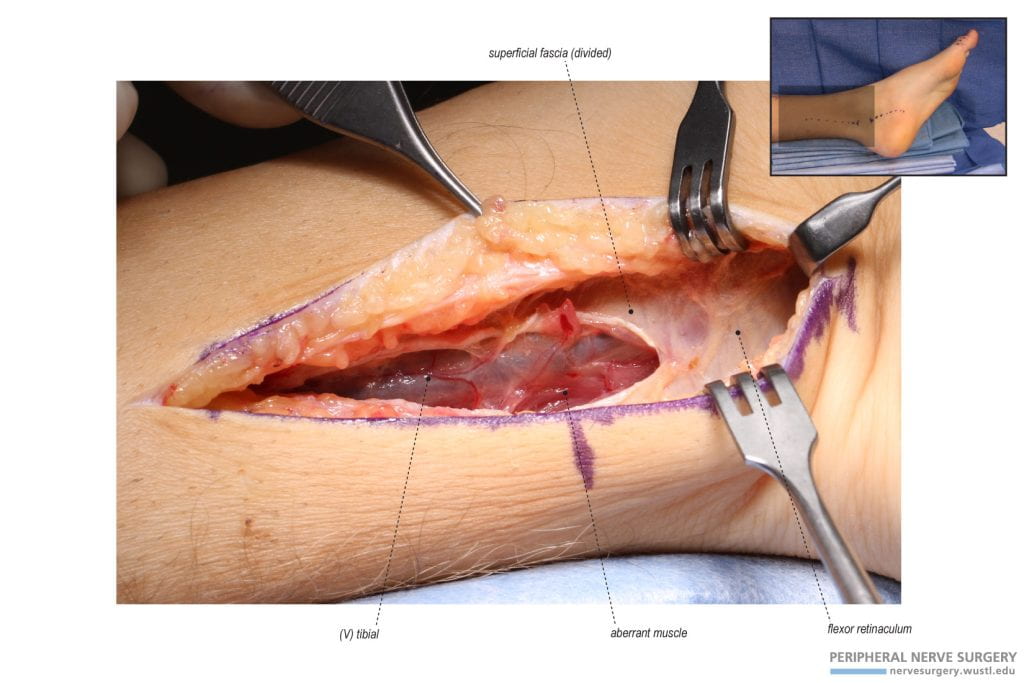
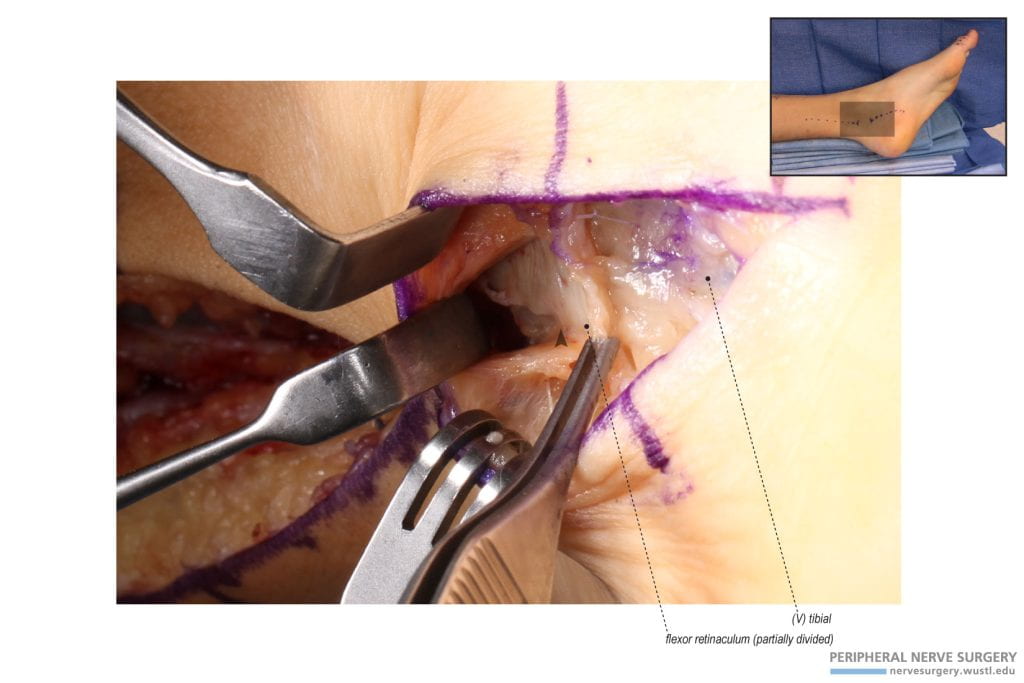
Figure 3 – Exposure and identification of the flexor retinaculum through the proximal incision. In the proximal incision, the exposure continues through the superficial fascia to identify the tibial vein. It is easier to first identify the “blue” vein than the “white” nerve. Deep to this vein, the tibial nerve is identified. In continuation and distal to the superficial fascia, the flexor retinaculum is identified. An aberrant muscle was present in this patient that was deep to the superficial fascia and flexor retinaculum. This muscle is divided during the case.
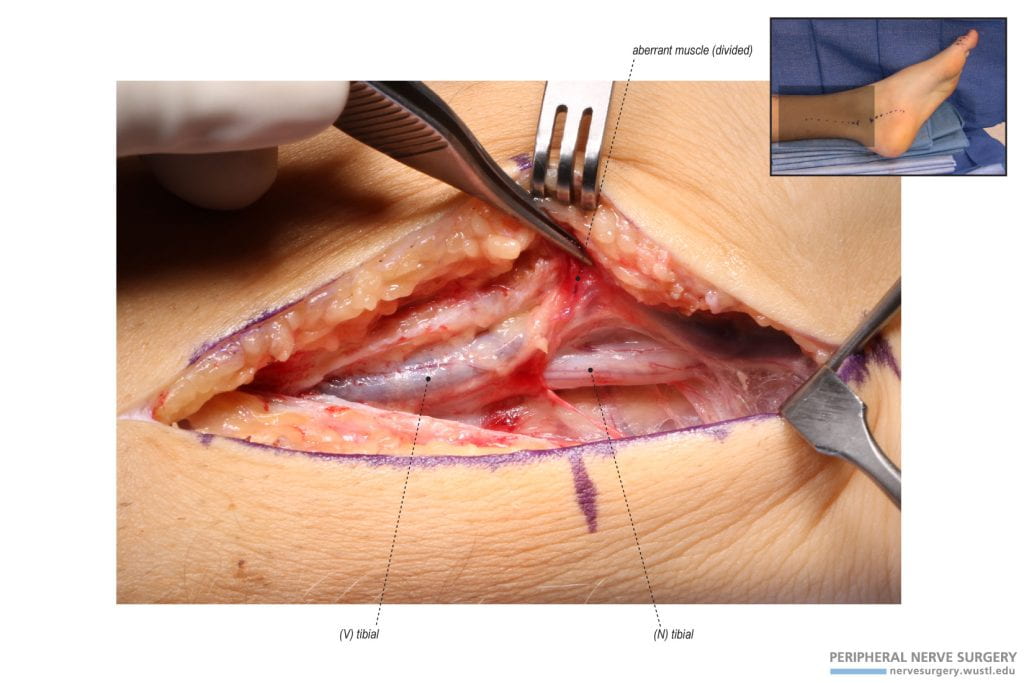
Figure 4 – Release of the proximal flexor retinaculum and identification of the tibial nerve. The flexor retinaculum is proximally divided as far distally as the exposure will allow. The distal release of the flexor retinaculum will occur through the distal incision. The tibial nerve is identified deep to the tibial vein.
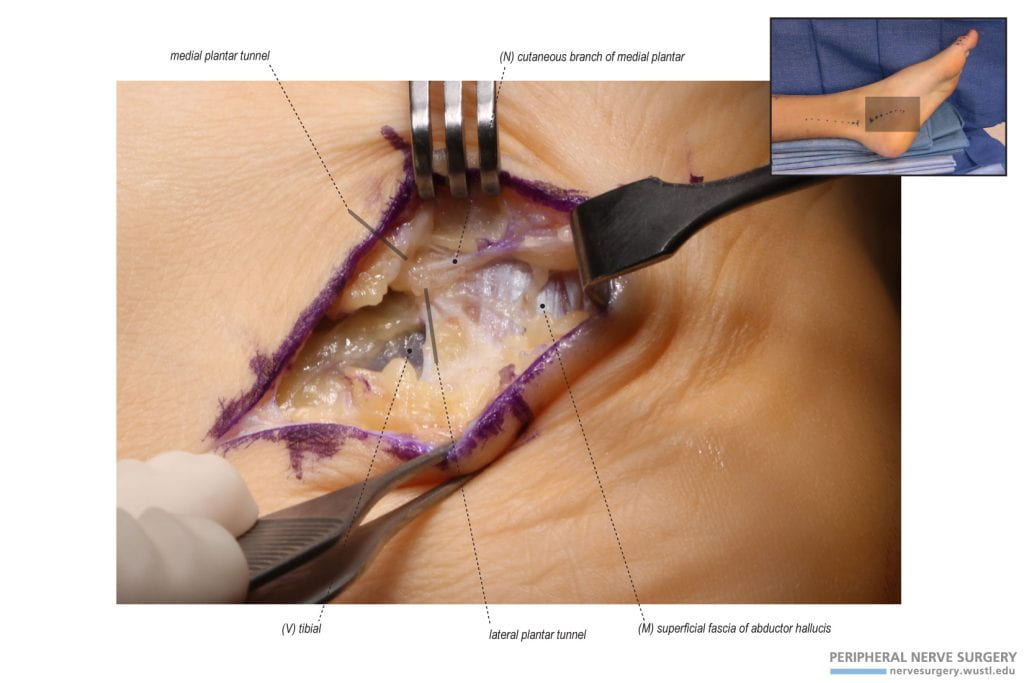
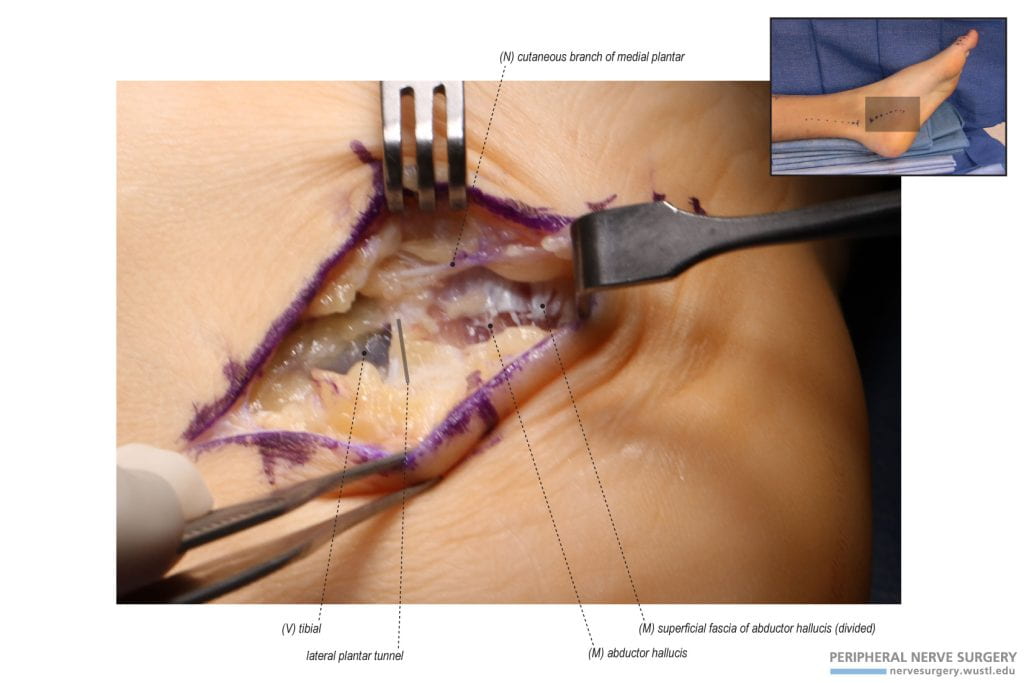
Figure 5 – Exposure and identification of the lateral plantar tunnel and the superficial fascia of the abductor hallucis. In the distal incision, a cutaneous branch of the medial plantar nerve is identified and protected upon exposure. The tendinous superficial fascia of the abductor halluies is identified. Proximal and deep to this muscle, the lateral plantar tunnel is identified with the course of the tibial vein. A septum is identified anterior to this tunnel and posterior to the medial plantar tunnel.
Figure 6 – Incision of the superficial fascia of the abductor hallucis. To expose the abductor hallucis, the tendinous superficial fascia is incised longitudinally along the course of the lateral plantar tunnel.
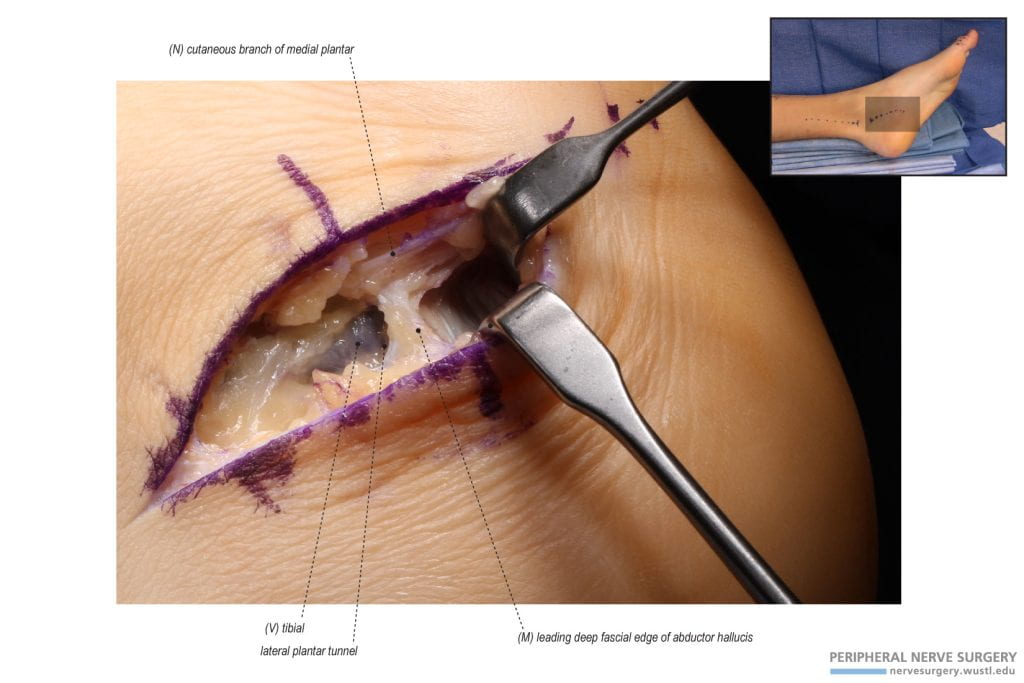
Figure 7 – Identification of the deep compressive fascia of the abductor hallucis. The abductor hallucis muscle is retracted distally and off of the deep fascia of the abductor hallucis to expose the tendinous leading edge of the lateral plantar tunnel. This tendinous fascia deep to the abductor hallucis is divided to decompress the lateral plantar branch of tibial nerve.
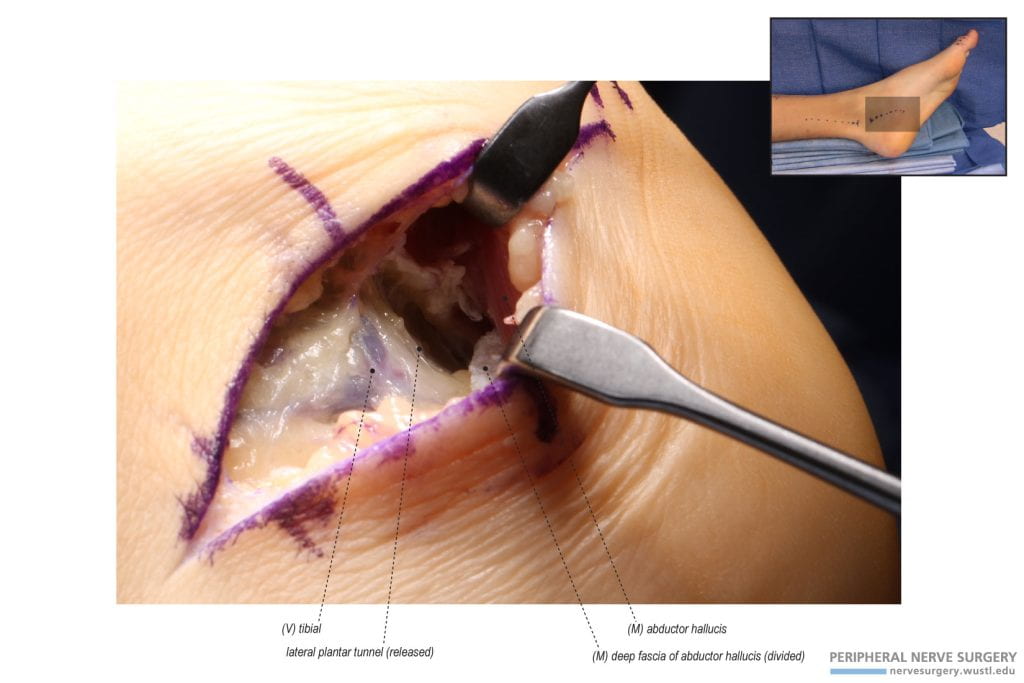
Figure 8 – Dividing the entire length of the deep fascia of the abductor hallucis. The deep fascia of the abductor hallucis is divided to expose the lateral plantar tunnel and decompress the lateral plantar branch of tibial nerve. This nerve is found deep to the tibial vein. The surgeon is looking distally down the tunnel and retracting distally.
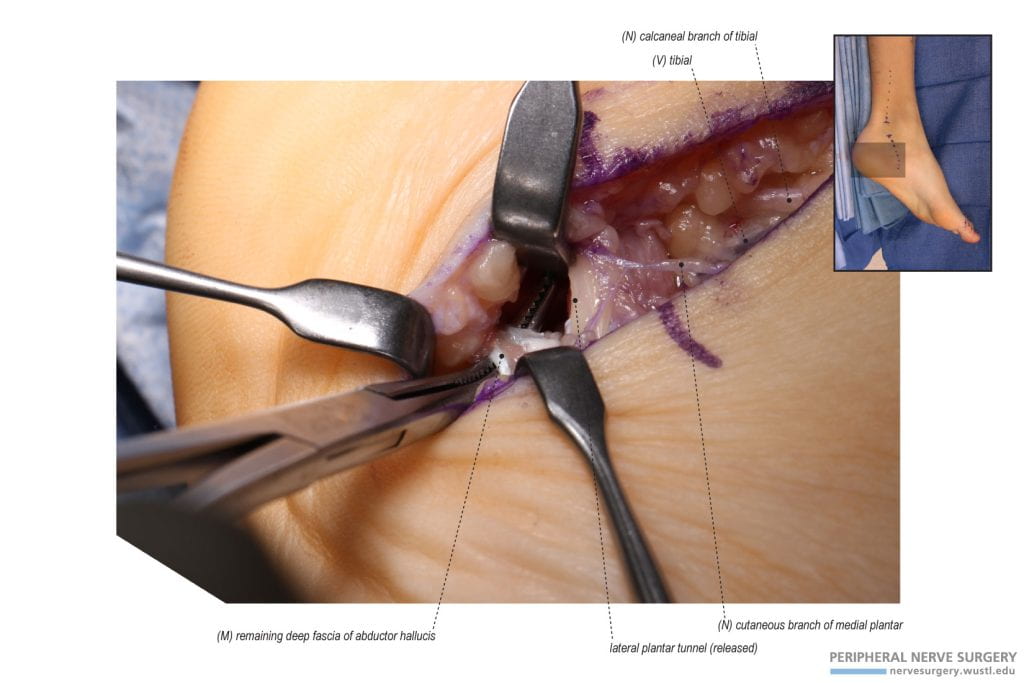
Figure 9 – Further division of the deep fascia of the abductor hallucis. Note the new orientation. The tendinous deep fascia of the abductor hallucis can extend distally and it is important to identify and release all components of this fascia. The remaining deep fascia of the abductor hallucis is identified and released. The surgeon is now looking proximally up the tunnel from the foot of the table while retracting proximally.
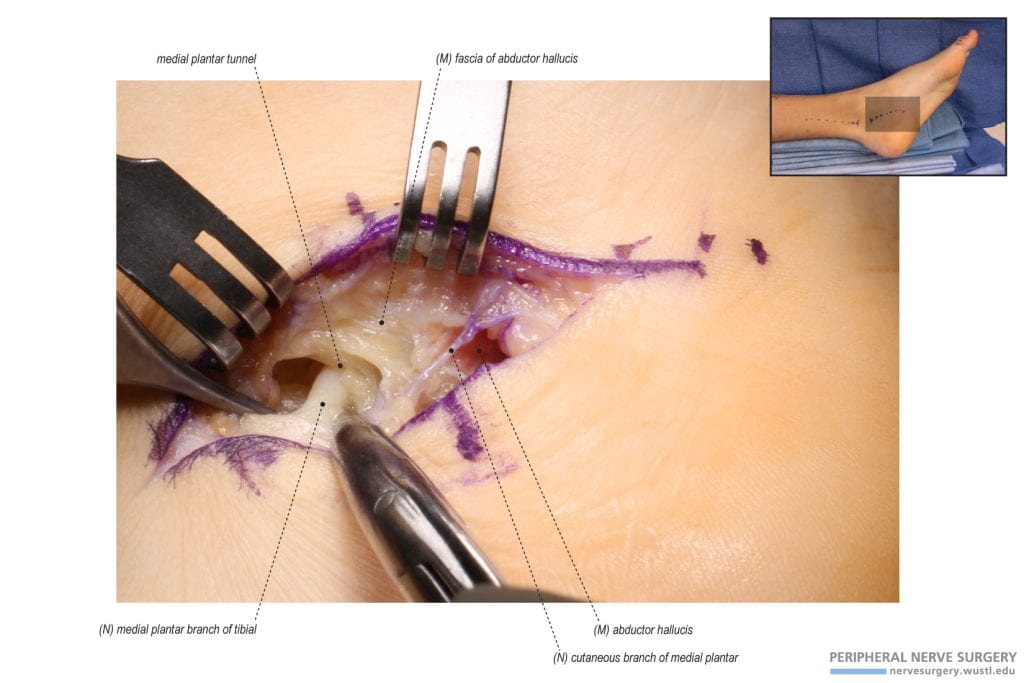
Figure 10 – Exposure and identification of the medial plantar tunnel and the fascia of the abductor hallucis. Note original orientation. The dissection moves anteriorly to identify the medial plantar branch of tibial nerve having a course deep to the tendinous fascia of the abductor hallucis through the medial plantar tunnel. A septum is identified posterior to this tunnel and anterior to the lateral plantar tunnel.
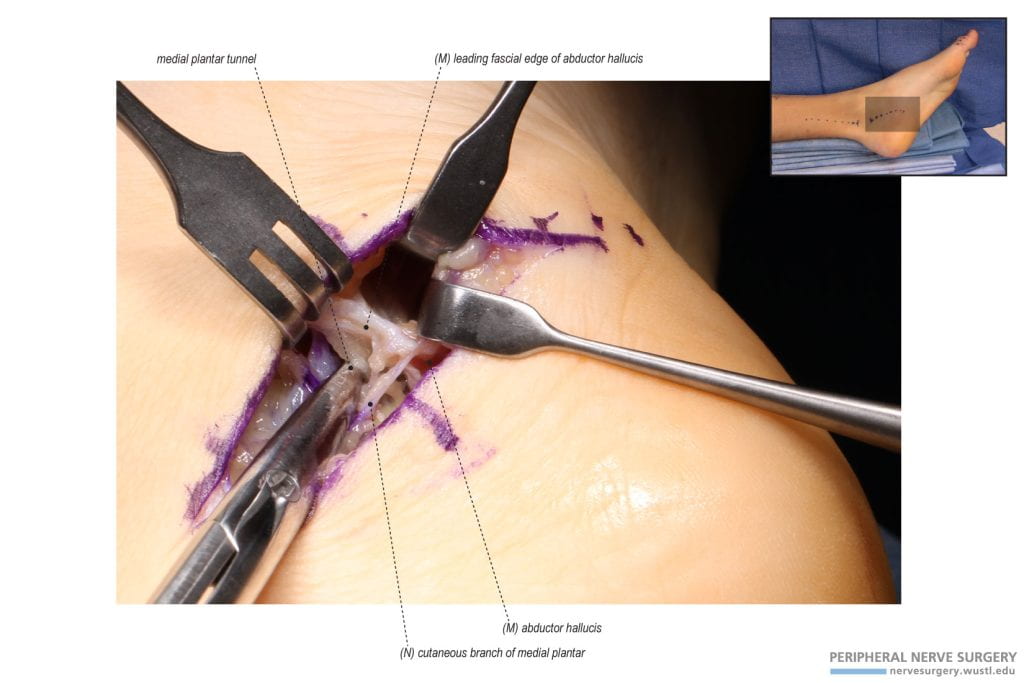
Figure 11 – Identification of the tendinous fascia of the abductor hallucis. The leading edge of the tendinous fascia of the abductor hallucis is identified superficial to the medial plantar nerve. This fascia is released to decompress the medial plantar branch of tibial nerve. The scissors are in the medial plantar tunnel and pushing up against the septum to orient the surgeon and correct tunnel.
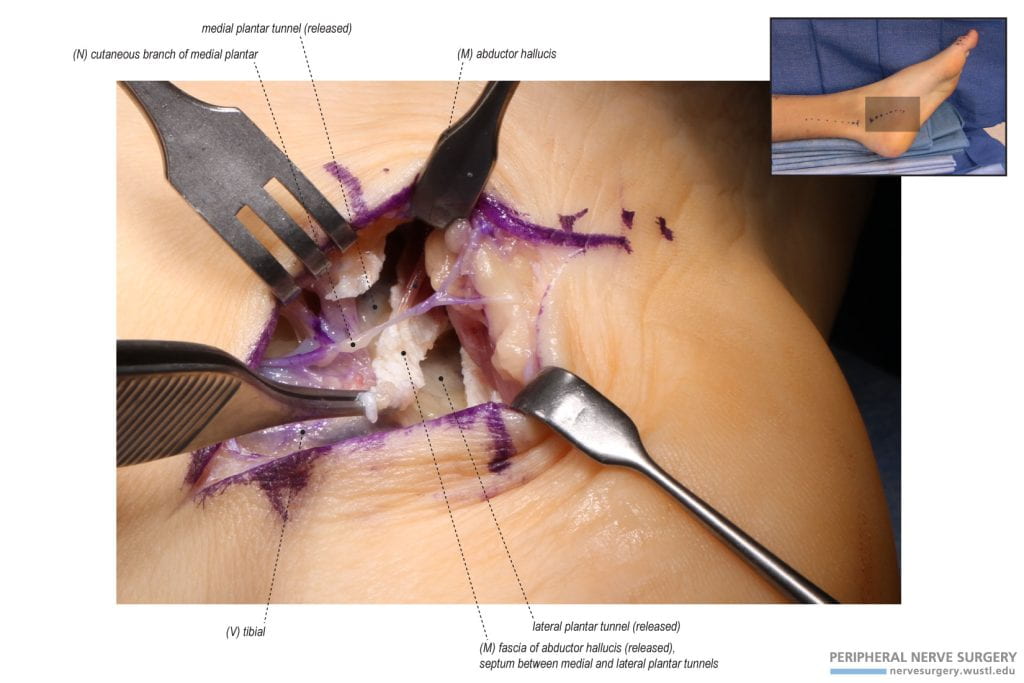
Figure 12 – Dividing the fascia of the abductor hallucis. The fascia of the abductor hallucis is divided longitudinally along the course of the medial plantar tunnel and as far distally as possible to release the medial plantar tunnel. This will decompress the medial plantar branch of tibial nerve. The septum that separates the medial and lateral plantar tunnels is seen.
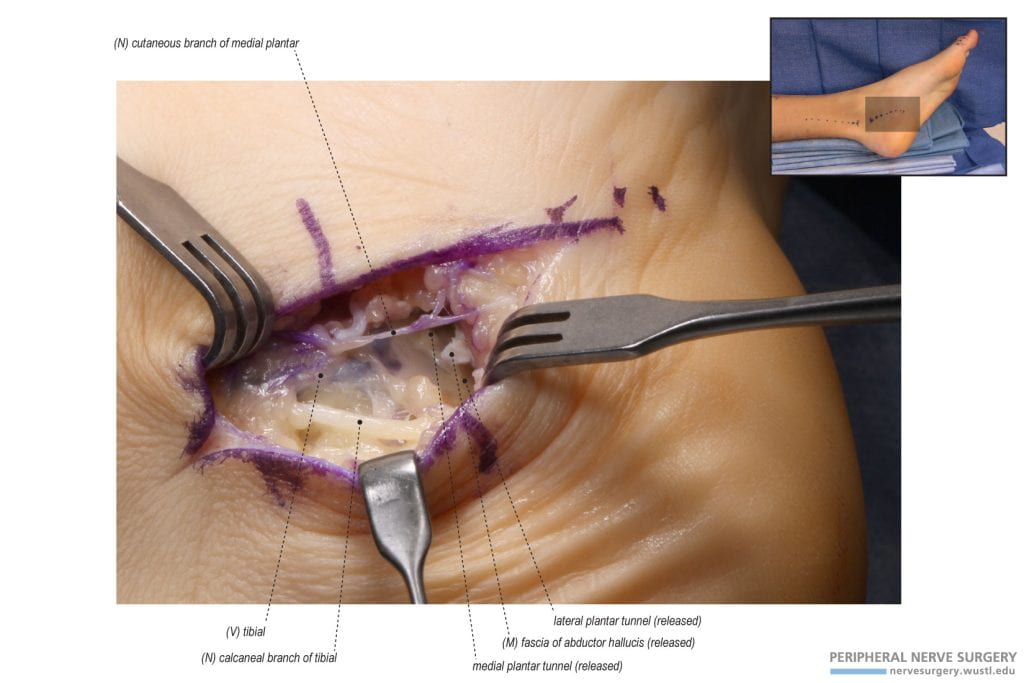
Figure 13 – Release of the calcaneal branch of the tibial nerve. Usually, the calcaneal branch of the tibial nerve will have a tunnel of its own. Release of the tunnel will decompress this cutaneous nerve. The calcaneal nerve branches from the tibial nerve proximally and posteriorly.
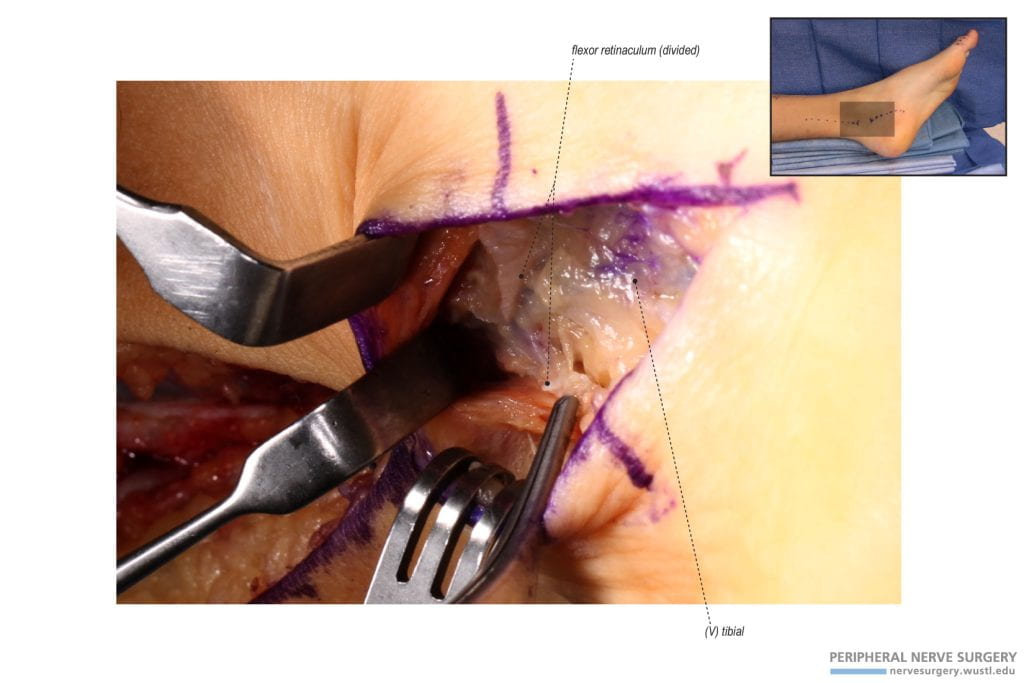
Figure 14 – Identification of the flexor retinaculum through the distal incision. The remaining distal component of the flexor retinaculum, which was not released from the proximal incision, is identified to make sure the retinaculum below the skin bridge is completed released.
Figure 15 – Release of the distal flexor retinaculum. The remaining distal component of the flexor retinaculum is released to decompress the tibial nerve deep to the tibial vein.